About two per cent of children aged under 10 years develop strabismus, a condition where the eyes do not line up in the same direction (often referred to as ‘lazy eye’, ‘cross-eyed’ or ‘squint’). Intermittent exotropia, where one or both eyes intermittently turn outward, presents in up to 70 per cent of cases.
 One of the most common non-surgical treatments for this type of strabismus is overminus lens therapy. This method involves prescribing additional minus glasses to their actual refraction to encourage the wearer to put extra effort in focusing their eyes, which in turn forces the eye muscles to bring the eyes into straight position.
One of the most common non-surgical treatments for this type of strabismus is overminus lens therapy. This method involves prescribing additional minus glasses to their actual refraction to encourage the wearer to put extra effort in focusing their eyes, which in turn forces the eye muscles to bring the eyes into straight position.
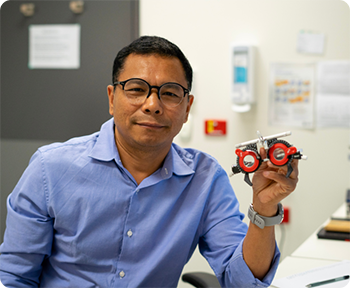
Queensland Children’s Hospital senior orthoptist Dr Jit Ale Magar, said despite being the most common type of strabismus, the pathophysiology behind intermittent exotropia was poorly understood.
“There are a lot of pathophysiological mechanisms responsible for the tendency of intermittently outward turning of the eyes. It may also be associated with disrupted coordination between the eyes and the brain.”
Dr Ale Magar To determine the best treatment method for intermittent exotropia, Dr Ale Magar’s team conducted a randomised clinical trial involving 132 children at the Queensland Children’s Hospital between 2018 and 2021.
Children aged four to 15 years who were receiving treatment at the hospital for intermittent exotropia, as well as patients referred from external practices, were randomly assigned to control and overminus groups. A novel algorithm was then developed to customise the optimised minus lens power for children in the overminus group. The algorithm encompasses all possible clinical factors responsible for the
strabismus. This is the first attempt to use such clinically plausible algorithm in calculating individualised doses of overminus lens in the treatment of intermittent exotropia.
 The results, published in Clinical and Experimental Ophthalmology in June 2022, showed the customised lenses prescribed through the novel algorithm were highly effective in controlling the deviation in intermittent exotropia.
The results, published in Clinical and Experimental Ophthalmology in June 2022, showed the customised lenses prescribed through the novel algorithm were highly effective in controlling the deviation in intermittent exotropia.
The trial also evaluated if overminus lens therapy in intermittent exotropia caused myopia (short sightedness). The results, published in British Journal of Ophthalmology in June 2022, found the therapy does not affect the natural course of how the eye grows and therefore, is safe.
Dr Ale Magar said the findings would have a significant impact among doctors and other eye care professionals who treat children with intermittent exotropia around the world.
“People are still working to get to the bottom of the condition and treatment,” he said.
“I want to continue working in this area so we can further improve the treatment outcomes for children.”
Dr Ale Magar The customised overminus lens calculation method is now embedded at the Queensland Children’s Hospital as the standard approach for prescribing overminus lens.
The ophthalmology team is now developing an online calculator using the algorithm so it can be used by practitioners everywhere.