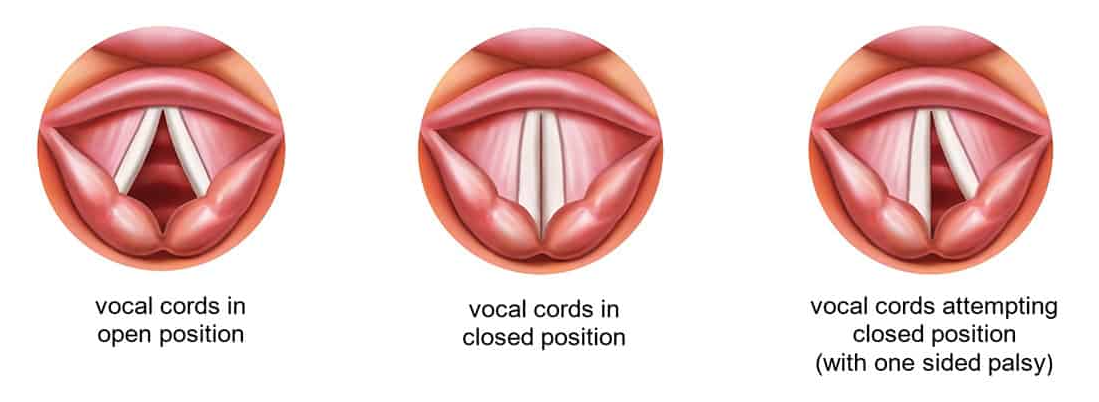
Vocal cord palsy is when the vocal cords can’t move or have weak or reduced movement on one or both sides. The vocal cords are 2 bands of tissue that are part of the voice box. They open to let air in and out when your child breathes and close together to produce sound used for speaking.
Vocal cord palsy happens when there is damage to the recurrent laryngeal nerve, this can happen:
- in childbirth
- in heart, lung or oesophagus surgery
- because of brain and nerve conditions and infections
- because of a mass in the neck, however this is rare.
In some children there is no identifiable cause, this is known as ‘idiopathic’ vocal cord palsy.
Signs and symptoms
The main signs and symptoms include:
- ‘squeaky’ or noisy breathing
- a breathy, weak voice
- a hoarse, quiet or silent cry in infants
- trouble eating - food or fluids may enter their windpipe or lungs when they swallow.
When to seek help
If your child has symptoms, see your GP.
If your child has a speech pathologist or ear, nose and throat (ENT) specialist, talk to them if you have concerns.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Diagnosis
If your GP thinks your child might have vocal cord palsy, they’ll refer them to an ENT specialist. An ENT will check your child’s vocal cords with a ‘scope’ to see how they’re moving. An ultrasound may also help see if there's reduced movement in either vocal cord.
Treatment
Most cases will get better without treatment. However your child may need help to prevent food or fluid going into their windpipe.
Your child may be referred to a speech pathologist for therapy. A speech pathologist can:
- guide your child through play-based exercises to help them control their breathing and use their voice effectively
- give you exercises to do with your child at home
- give you strategies to keep your child safe while eating and drinking
- teach you how to stop fluid or food entering your child’s airway during breast or bottle feeding, or while eating and drinking.
Developed by the Speech Pathology Department, Queensland Children’s Hospital. We acknowledge the input of consumers and carers.