It’s common for children with Spina bifida to experience incontinence — this means they may have trouble controlling their urine and bowel movements. This is because Spina bifida affects the nerves from the spinal cord that supply muscle control and sensation to your child’s bladder and bowel. The result is called ‘neurogenic bladder and bowel’ and affects your child’s voluntary bladder and bowel functions partially or completely.
Managing urinary incontinence
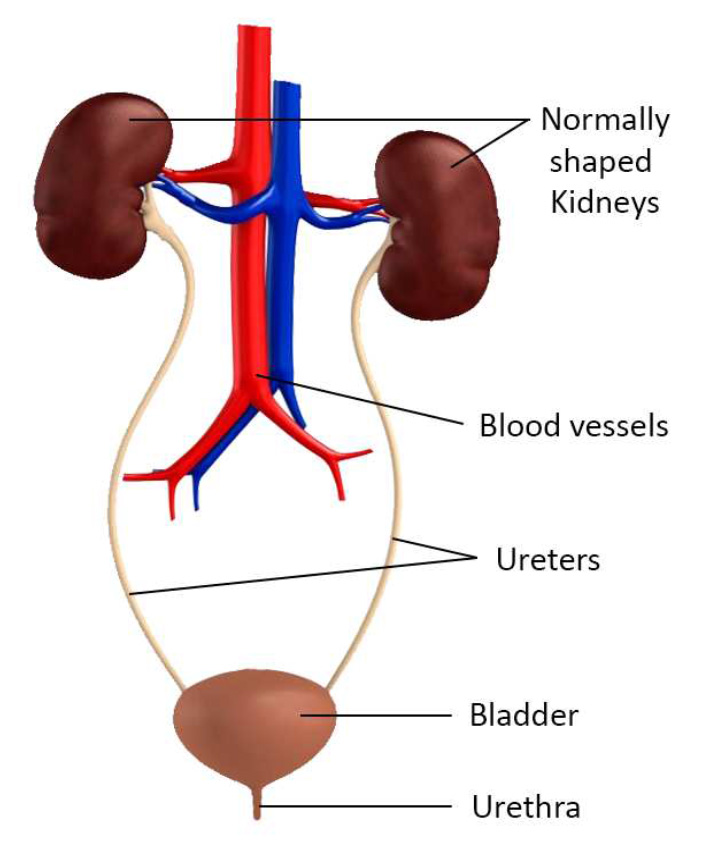
Your child’s urinary system is important for balancing water and electrolytes in their body, filtering toxins and excess water from their blood to form urine and returning salt and other important elements to the blood. The system is also made up of several parts, including 2 kidneys, 2 ureters, a bladder and a urethra. With so many features and functions, it’s important to keep your child’s urinary system as healthy as possible by:
- protecting the kidneys by preventing reflux of urine
- reducing urinary tract infections (UTIs)
- ensuring they can urinate in a socially acceptable and hygienic way.
This can be done through a combination of:
- Clean Intermittent Catheterisation
- medications to relax the bladder muscle
- a toilet timing and training program for regular toileting
- adaptive clothing and continence products (e.g., continence underwear, pads)
- surgical procedures
- regular check ups
- drinking plenty of water.
Clean Intermittent Catheterisation (CIC)
The key to a healthy urinary system and protecting the kidneys is frequent and complete bladder emptying.
Clean Intermittent Catheterisation (CIC) is a clean method of draining your child’s bladder several times a day (usually every 4 hours during waking hours) with a catheter using a clean but non-sterile technique. A catheter is a flexible tube that drains urine from the bladder into a toilet or collection container. It helps completely empty the bladder, reducing urinary leakage and protecting the kidneys from damage.
Children with Spina bifida are often introduced to CIC at birth and start learning to perform the procedure on their own by kindergarten or preschool. Children can perform parts of the procedure from 4-5 years old, and most children can be reasonably independent by 8 years of age. Even if your child becomes proficient with the CIC process, they should still see their urologist or paediatrician regularly to monitor kidney and bladder function.
Urinary Tract Infections
A Urinary tract infection (UTI) is a bacterial infection in the urinary system. Children with a neurogenic bladder are at a higher risk of urinary tract infections because their bladder isn’t emptying properly or completely. Urine sitting in the bladder for long periods can cause infection.
Some children have kidney reflux due to high pressures in the bladder or a thick bladder wall, and kidney reflux puts children at high risk for urinary tract infections too.
Catheterising can be protective against urinary tract infections as it helps to empty the bladder and reduce the pressures on the urinary system.
Urinary tract infections are important to treat if they are causing symptoms. Untreated urinary tract infections can make someone very sick and can also potentially lead to irreversible kidney damage, so know the symptoms to look out for:
- fever, chills, shakes
- cloudy or discoloured urine
- strong smelling urine
- blood in the urine
- pain in the back or abdomen
- pain on urination (burning or stinging)
- headache, fatigue
- nausea, vomiting, decrease appetite
- increased frequency and need to urinate, or episodes of wetting between catheters if normally dry.
Treating UTIs can include:
- antibiotics
- increasing water intake
- increasing frequency of CICs
- nurse review of your catheter type and your technique.
It’s important to remember that bacteria can still live in your child’s bladder without causing any symptoms. This is called bacterial colonisation. If your child’s urine sample reveals bacteria but they have no symptoms, avoid using antibiotics. Overusing antibiotics may lead to future UTIs growing resistant and more difficult to treat.
Monitoring your child’s urinary system
Monitoring your child’s urinary system regularly is important for maintaining kidney health. Ultrasounds will be scheduled within the first week of life and then at:
- 6 weeks
- 3 months
- 6 months
- every 6 months until 3 years old.
We recommend yearly ultrasounds for children over 3 years old, and monitoring should continue throughout their life.
Managing bowel continence
The body needs to rid itself of waste products or it will become very unwell. The bowel removes the waste from the lower digestive system. The bowel consists of the small intestine, the large intestine, the rectum, internal and external anal sphincters and anal canal.
Bowel problems, especially constipation and bowel incontinence, are common in people living with Spina bifida. Bowel problems are the result of damaged nerves at the bottom of the spinal cord. Nerve damage generally affects the external anal sphincter, the sensory mechanism which tells the brain that the rectum is full, and the muscles which move the faeces along the colon and out of the body.
Bowel incontinence can be managed with:
- a high fibre diet with plenty of water and fluids
- medication to soften the stools and stimulate bowel movements
- a toilet timing and training program.
- enemas and bowel washouts
- manual evacuation
- continence aids
- incontinence underwear and swimwear
- exercise
- surgical procedures
- regular checkups.
Management of constipation is very important in both treatment and prevention of incontinence.
Bladder and bowel continence at school
Starting school can be a daunting time for all children. For children with Spina bifida and neurogenic bladder, this can be an even more challenging time. We recommend all parents make time to speak with their child’s school before the school year begins to discuss their child’s specific needs. This will include discussion regarding toileting to ensure continence is maximised with safety and dignity.
We recommend working with school staff to develop a management plan that includes the following elements:
- Encouraging your child to drink water regularly (e.g., allow them to keep a water bottle on their school desk).
- What to do when accidents occur at school (e.g., storing spare clothing and continence aids).
- Access to suitable facilities. This may include clean toilets and facilities with a wheelchair accessible sink, bin and cupboard for storing consumables.
- A school toileting routine established with consideration to additional time required and/or requirements for aid support for toileting or catheterisation assistance.
Preventing accidents during exercise
Continence can be tricky during physical activity because movement helps bowels work better and this can lead to accidents during exercise. It’s important to set up preventative toilet routines around exercise to ensure your child continues to associate physical activity with fun.
Here are some tips to help reduce the anxiety and likelihood of accidents during physical activity.
- Ideally, empty bowels prior to exercise, either the night before or morning of expected activity.
- Immediately before the activity, encourage your child to sit on the toilet and push, rock, cough or laugh to empty faeces from the bottom part of the bowel.
- Consider taking an additional catheter for CIC before exercising.
- Pack extra continence aids to be within reach during activity.
Becoming Independent
Becoming independent with a neurogenic bladder and bowel may seem challenging, but even the smallest step in the right direction can help your child’s confidence in themselves. Start with steps such as independent handwashing, undressing and dressing or transfers onto and off a toilet. Then progress to discussing the correct sequencing and timing of their daily activities. As your child matures and becomes more confident, allow them to take more responsibility of this self-care task.
When to seek help
See your GP if your child experiences pain or discomfort when toileting or displays any symptoms that indicate a UTI.
Present to your local emergency department if any symptoms appear serious or get worse.
If it's not an emergency but you have any concerns, contact Spinal Disabilities Team on 3068 2736 or CHQ.spinaldisabilities@health.qld.gov.au
For more information
- What is Spina bifida?
- Common health issues in children with Spina bifida
- Sacral agenesis
- Spina bifida and associated pain
- Spina bifida and skin care
- Spinal cord detethering
- Constipation
Images courtesy of Spina Bifida & Hydrocephalus Association Qld (no longer in operation)
Developed by the Queensland Paediatric Rehabilitation Service, Children’s Health Queensland’s Child Health Service. We acknowledge the input of consumers and carers. Resource ID: FS401 Reviewed: June 2024
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.