Pre-school wheeze (also called reactive airways disease or viral-induced wheeze) affects the airways (the tubes that carry air from the mouth and nose to the lungs) of children aged 1 to 5 years.
It happens when your child’s airways become swollen and fill with mucous, making it hard for them to breathe.
Wheeze is mostly caused by viral infections but can also be caused by changes in weather (from warm air to cold air), dust mites and cigarette smoke.
A doctor can diagnose pre-school wheeze by listening to your child’s chest and understanding their symptoms.
Most children with pre-school wheeze will not go on to develop asthma in later life.
Signs and symptoms
- Wheezing sound (a whistling sound when breathing in and out)
- Fast breathing and/or difficulty breathing
- Muscles of the chest drawing in when breathing
- Cough
Treatment
Pre-school wheeze is treated with medicine which is usually inhaled (breathed in) so it goes straight into the lungs. Medicines include relievers and steroids.
Relievers (e.g. Ventolin, Asmol, Bricanyl)
Your child should use a reliever as soon as they have the asthma symptoms or before they exercise (if directed by your child’s doctor). Relievers:
- are used during an attack
- give quick relief from asthma symptoms
- work quickly and the effects can last up to 4 hours
- are available in pharmacies. You won’t need a prescription.
Steroids (liquid)
Your child should take this as directed by your doctor. Steroids:
- can treat asthma symptoms
- can take several hours to take effect
- are available in pharmacies. A doctor’s prescription is needed.
Your doctor may provide a Pre-School Wheeze Action Plan which explains how and when your child should take their puffer medication.
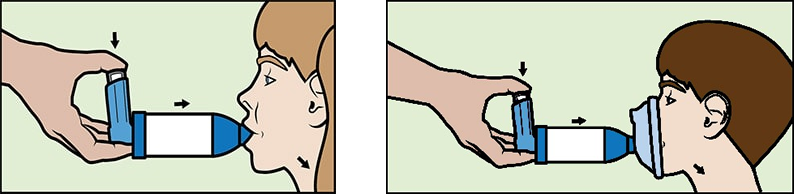
Children should always use a spacer to inhale their puffer medication. A spacer is a cylinder-shaped object that helps the medicine go straight into your child’s lungs. If your child is having a hard time using the spacer with their lips, they may have to use a mask.
Care at home
Pre-school wheeze can be treated at home by:
- following the Pre-school Wheeze Action Plan prepared for your child by their doctor (keep it in a safe place).
- keeping your child away from cigarette smoke
- making sure your child always has their puffer and spacer (and mask, if required) with them
- sharing your child’s Pre-school Wheeze Action Plan with anyone who cares for your child (e.g. relatives and teachers).
If you have any concerns about your child’s condition, call 13 HEALTH (13 43 25 84) to speak to a registered nurse 24 hours a day, seven days a week for the cost of a local call. Ask for an interpreter if you need one.
When to seek help
See your GP if your child has any common symptoms or if they:
- wake up at night with wheezing
- are using the reliever at least every 3 hours for more than 24 hours.
Your child should have regular check-ups with their doctor as symptoms and medicine may change. If your child has been in hospital with pre-school wheeze, they should see their doctor within 1 week of going home.
In an emergency, call Triple Zero (000) and ask for an ambulance. Seek help immediately and continue using the reliever if your child has:
- trouble breathing or talking
- blue lips
- symptoms that get worse very quickly.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
More information
Watch our asthma education videos.
Developed by Emergency Department, Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS319. Reviewed: July 2022.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.