Patent ductus arteriosus (PDA) is a congenital (present at birth) heart defect found in the days or weeks after birth.
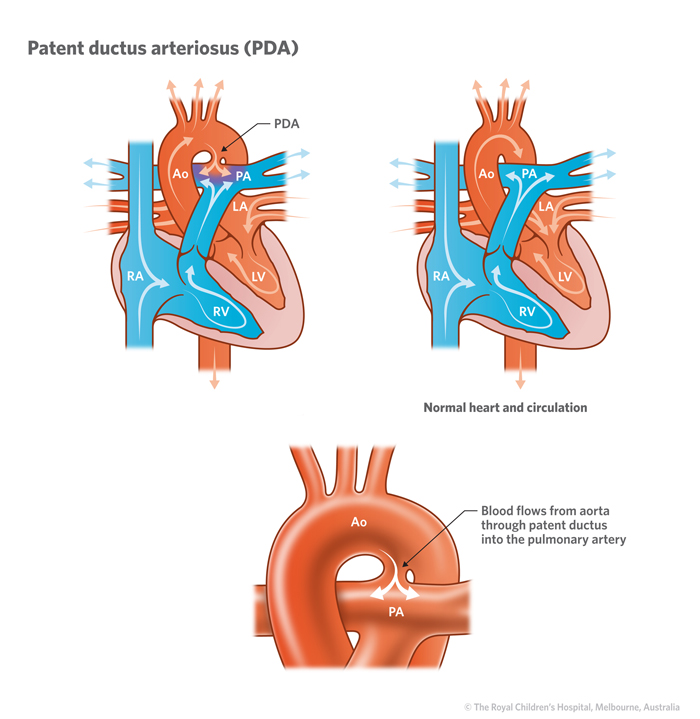
Before a baby is born, the ductus arteriosus (a blood vessel) allows blood to go directly to the aorta, bypassing the pulmonary arteries (lung vessels) and lungs, then onto the placenta to collect oxygen and nutrients. After birth, when the placenta is gone and the baby breathes, the ductus arteriosus is no longer necessary, and should close.
When the vessel fails to close after birth, it is called a PDA. When the PDA remains open, blood can flow from the aorta back into the pulmonary arteries. This extra blood flow to the lungs creates a turbulence in the blood vessel and if the PDA is large can result in heart failure.
In some congenital heart defects, PDA allows blood to get into the lungs if the usual pathways are absent or obstructed.
Signs and symptoms
Children with small PDAs can have no symptoms but can be at risk of bacterial infection of the duct (infective endocarditis).
Babies and children with larger PDAs may have the following signs and symptoms:
- fatigue when feeding/playing
- poor weight gain and growth
- shortness of breath and rapid breathing
- sweating during feeding
Diagnosis
A doctor may suspect a diagnosis of PDA if they hear a heart murmur and will refer a child to a paediatric cardiologist. A murmur is heard when blood becomes turbulent as it travels through an obstructed area.
A cardiologist will typically perform a range of tests, including:
- electrocardiogram (ECG) will measure the electrical activity of the heart.
- echocardiogram (Echo) that uses sound waves to produce a picture of the heart.
- cardiac catheterisation , which measure pressures and oxygen levels, and creates images of heart structures using X-ray equipment. The procedure is performed under a general anaesthetic.
Treatment
A PDA that creates a murmur and/or is causing symptoms may require medical treatment or surgical repair.
In premature babies, a PDA can sometimes be closed with medications such as indomethacin and ibuprofen.
Some PDAs can be closed in babies and children using a device during cardiac catheterisation. This procedure is less invasive than surgery and usually only requires 1-2 days in hospital. It requires general anaesthesia and catheters (thin flexible tubes) which are usually inserted into both an artery and a vein at the top of the leg during the procedure.
Surgical repair of a PDA involves ligating it (tying a suture around it) or stitching it closed.
Developed by the Queensland Paediatric Cardiac Service, Queensland Children’s Hospital.
Resource ID: FS243. Reviewed: October 2023. Illustrations courtesy of the Royal Children’s Hospital Melbourne.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.