Warfarin is an anticoagulation medication, sometimes known as a “blood thinner”, which is prescribed to:
- Treat a blood clot that has been found inside a blood vessel to ensure the clot does not increase in size or break off and move to another part of the body, or
- Prevent a blood clot as the doctor thinks the person has a higher risk than other people of forming a blood clot.
Patients may need to take warfarin after mechanical heart valve replacement or other surgical procedures (eg Fontan) and for management of cardiomyopathy and rarely, arrhythmia. It is also used for other conditions where blood thinning is required.
There are two brands of warfarin: Coumadin® and Marevan®. The two brands are not interchangeable so you must only take the brand that your doctor prescribes. The brands have different coloured tablets according to their strength to make it easier to avoid mistakes with the dose.
You may be given more than one strength of warfarin to allow you to make dose changes. Make sure you are giving the correct tablet by checking the colour and the strength.

The brand of warfarin supplied for your child is:_________________
While using warfarin – Remember
- There is a risk of bleeding – tell all your doctors, dentist and other health professionals that warfarin has been prescribed
- Do not stop taking warfarin unless advised to do so by your Treating Team
- Many medicines and foods interact with warfarin and may prevent it working as well or increase the risk of bleeding
- Regular blood tests are needed
- Keep using the same brand of warfarin (do not change brands)
Giving my child warfarin
The dose of warfarin will be determined by your Treating Team based on regular blood tests and your child’s current condition.
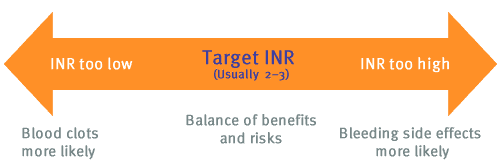
Regular blood tests are required to monitor how well warfarin is working. The International Normalised Ratio (INR) measures the time it takes for your blood to clot, aiming for a safe balance so blood doesn’t clot too fast or too slow. The INR result is used to adjust the warfarin dose.
Your child will be given a target INR range depending on the reason they have been prescribed warfarin.
When warfarin is first started the INR test may need to be done every 1-2 days until it is in the target range. Then testing is gradually spread out over time to ideally every 2-4 weeks.
Many different things affect warfarin therapy and it will often take 2-4 days before this will be reflected in the INR going up or down.
Diet: Vitamin K (phytomenadione) is found in food and drinks. It is in high amounts in green vegetables. Vitamin K stops warfarin from working properly. You don’t need to avoid Vitamin K-rich items. Instead, eat or drink them consistently in the diet.
Babies who are exclusively breast-fed (which does not contain Vitamin K) are very sensitive to warfarin so your Treating Team need to be made aware of this. Let them know if your baby’s feed is changed or topped up with formula.
Infant formula or supplementary milk formulas (e.g. Sustagen) have additional Vitamin K in them so if the formula or amount of supplements your baby or child has each day changes let your Treating Team know.
Illness: Some illness can affect warfarin therapy, colds usually don’t however if your child is unable to eat/drink or has vomiting/ diarrhoea for more than 24 hours please contact your Treating Team. An INR test may need to be done sooner than planned.
Surgery and medical procedures: Tell all medical professionals doing surgery or medical or dental procedures that your child takes warfarin and is at risk of bleeding. They may request to withhold or delay the warfarin for your child, and you may need to be given a different medicine to cover your clotting risk while warfarin is not used. This needs to be checked with your Treating Team. Let your Treating Team know about planned procedures, even if the doctor doesn’t want to change the warfarin.
Alcohol: The INR can go up quickly with alcohol consumption. Alcohol consumption is not recommended in children under 18 years of age. The Treating Team need to know if this is going to happen so that a plan can be made to keep your child safe.
Sport and Activity: Contact sports and those with risk of serious injury (e.g. football, karate, hockey, basketball, soccer, gymnastics, alpine skiing, boxing) should be avoided due to the increased risk of bleeding while taking warfarin. When involved in activities where there is a high risk of falling (e.g. cycling, skateboarding, rock climbing) a helmet should be worn.
Weight-bearing exercises (e.g. tennis, walking, dancing) are very beneficial in helping to strengthen bones and should be encouraged. If you have queries about the safety of an activity you can discuss this with your Treating Team.
When and how should I give warfarin?
Warfarin should be given at the same time each day usually in the evening, so that dose changes based on blood tests can be started the evening of the same day.
Tablets should be swallowed with a glass of water, or similar liquid (take care with grapefruit juice). Tablets can be cut in half or dispersed in a liquid to be given via mouth or feeding tube. Your pharmacist can provide you with details on how to administer dispersed or partial tablets.
What to do if a dose is missed or my child vomits
- Give the missed dose when you remember, so long as this is less than 4 hours since the dose was due. If it is more than 4 hours since the dose was due, then don’t give the dose and restart at the usual time the next day and contact your Treating Team as soon as you can during business hours.
- Never give a double dose of the medicine.
- If your child vomits less than 30 minutes after having a dose of warfarin, give them the same dose again.
- If your child vomits more than 30 minutes after having a dose of warfarin, you do not need to give them another dose. Wait until the next normal dose.
- If your child vomits again, seek advice from your Treating Team. They will decide what to do based on your child’s condition and the specific medicine involved.
What to do if I give too much warfarin
If you think your child has had too much warfarin call the Poisons Information Service on 13 11 26 even if your child shows no effects. In an emergency, call 000 for an Ambulance or take your child to hospital straight away. Have the medicine packaging with you, even if it is empty, as this information will be useful.
What about using other medicines with warfarin?
Tell your doctor or pharmacist about any other medicines or products your child takes before starting warfarin as they may affect the warfarin. This includes prescription, over the counter medicines, vitamins, supplements, herbal or complementary medicines that you buy from a pharmacy, supermarket, health food shop or online. Always tell the treating team or pharmacist when medicines are started, stopped or when doses change. It may be necessary to do an INR test sooner than planned to check the INR is in the target range.
You can give your child medicines that contain paracetamol (to treat pain and fever), unless your doctor has told you not to.
Aspirin, anti-inflammatories such as ibuprofen, and herbal medications must be avoided while on warfarin (unless advised differently by your doctor).
Tell all healthcare professionals you see – your doctor, dentist, physiotherapist, podiatrist, alternative health practitioner and pharmacist – about all medicines your child is taking before starting any new medicine.
Possible side effects – what other effects can occur?
Side effects you must do something about
Bruising and bleeding are the main side effects of warfarin , however when warfarin is taken correctly, and the INR is kept in the target range, bleeding is uncommon.
Contact your Treating Team straight away (or out of hours take your child to a hospital or call 000 for an ambulance) if you see any of the following:
- If your child falls or suffers a blow to the head, even if they do not lose consciousness, blank out or have a headache
- Significant bruises or tender swellings without obvious cause
- Nose bleeds that don’t stop after 20 minutes despite local measures of pressure and ice
- Blood in urine, poo, vomit or coughed up
- Severe headache or back pain
- Swelling and pain in the stomach
- Very heavy menstrual periods
- Prolonged bleeding from small cuts
Other side effects you need to know about
Females of child bearing age/potential on warfarin should use reliable contraception as birth defects can occur if women fall pregnant while taking warfarin. If your child becomes pregnant or is planning to, this should be discussed with your Treating Team so that an alternative therapy can be discussed.
Possible long term side effects
If your child is on warfarin for more than 12 months a bone mineral density scan (type of x-ray) may be requested to monitor the strength of the bones as osteoporosis can occur with long term therapy. For this reason, eating and drinking calcium (dairy) rich foods and participating in weight-bearing exercise can assist in maintaining bone strength.
There may be other side effects not listed above. If you notice anything unusual and are concerned, contact your doctor.
General medicine advice
Only give this medicine to your child who was prescribed it. Never give it to anyone else, even if their condition appears to be the same, as this could do harm. Contact Poisons Information Centre on 13 11 26 if another person takes this medicine.
Always have valid prescriptions and enough supply of warfarin.
Store warfarin, in a cool dry place away from heat, direct sunlight and moisture, below 25oC. Dispose of expired medicines or medicines you no longer need to your pharmacy.
Store all medicines out of sight and where children cannot reach them. Always keep medicine in the container or box that it came in.
For more information
- Warfarin patient education booklet – Viatris – available where your tablets are supplied
- This fact sheet is about using this medicine in children and young people. Some information may be different from the manufacturer’s Consumer Medicine Information (CMI). The manufacturer’s CMI is found at NPS MedicineWise. These should be read together.
- Talk to your doctor, nurse or pharmacist.
Contact us
In an emergency, always contact 000 for immediate assistance
Haematology Service
Monday-Friday (8am-4pm)
Haematology Nurse
t: 0457 719 233
Doctor (Registrar)
t: 07 3068 4562
After hours, weekends and public holidays
Contact the Queensland Children’s Hospital switch and ask for the Haematology Consultant On-Call
t: 07 3068 1111
Queensland Paediatric Cardiac Service
Monday-Friday (8am-4pm)
Care coordinator
t: 07 3068 2362 (voicemail)
After hours, weekends and public holidays
Contact the Queensland Children’s Hospital switch and ask for the Cardiology Fellow On-Call
t: 07 3068 1111
Pharmacy Department
Level 2, Queensland Children’s Hospital 501 Stanley Street, South Brisbane 4101
t: 07 3068 1901 (Monday to Friday 9am – 5pm, Saturday, Sunday and Public Holiday 9am – 12 midday)
Endorsed by Queensland Children’s Hospital Medication Safety Committee and developed by Haematology and Queensland Paediatric Cardiac Service with input from parents and carers.
Document ID: CHQ-MFS-75701. Updated: 21/8/2023 v2.0.
Contact CHQMedicationSafety@health.qld.gov.au for sources used to create this Fact Sheet.
Disclaimer: We take great care to make sure the information in this Fact Sheet is correct, up-to-date and reflects current use in Australia. However, medicines can be used in different ways for different patients. It is important that you ask the advice of your doctor or pharmacist if you are not sure about something.
This Fact Sheet is to be used as an aid, rather than a substitute for a discussion with your doctor or pharmacist. Children’s Health Queensland Hospital and Health Service accepts no responsibility for any inaccuracies, omissions, reliance placed, or the success of any treatment regimens detailed in this Fact Sheet.