What is a cleft palate?
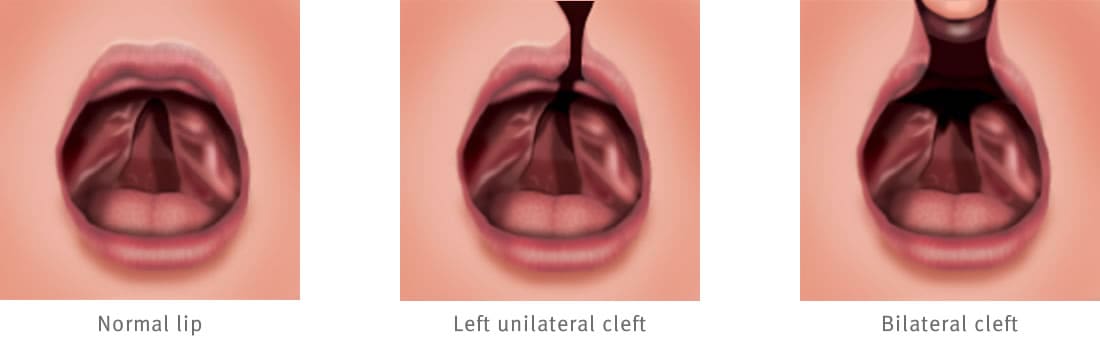
A cleft palate is when the palate fails to develop properly, causing a gap between the roof of the mouth and the floor of the nose. It can involve a hard and soft palate, the soft palate only, or the muscles of the soft palate only. The child may also have a cleft lip.
Why does it happen?
The cause of a cleft palate is unknown. It can be genetic, and sometimes multiple members of the same family are born with cleft palates. Other times, there is no family history.
Diagnosis
Pre-birth
If the cleft palate is picked up in a pre-natal scan, you can organise to talk to a cleft/craniofacial clinical nurse to give you some general information and answer any questions you may have.
Post-birth
Most babies with a cleft palate are unable to create enough suction to draw the necessary amounts of milk easily from the breast, or a bottle. Establishing feeding can be a problem and may mean you stay longer in hospital before discharge. Feeding problems can usually be solved by using teats and bottles specially designed for babies with cleft palates. Your speech pathologist will help prescribe the feeding equipment to best establish feeding. A cleft nurse will contact you in the first few weeks following the birth. An appointment will be made for you and your baby to attend a multidisciplinary cleft clinic at the hospital. The cleft clinic team includes a plastic and reconstructive surgeon, dental specialist and speech pathologist. Your child may also be referred to a paediatrician, ear nose and throat (ENT) surgeon, and an audiologist.
What is the treatment?
Surgery
A plastic and reconstructive surgeon from the cleft team will surgically repair the gap in the palate. The surgery usually takes between two to six hours, depending on the type of cleft palate repair your child needs. Generally, cleft palate repair uses the existing tissue at the sides of the palatal gap in the roof of the mouth and the floor of the nose to reconstruct the centre of the palate. The soft palate muscles are then released from their abnormal position and relocated and repaired to create a sling of muscles within the soft palate. This enables elevation and lengthening of the soft palate to create speech sounds, and to stop food and fluid regurgitating through the nose.
The repair usually takes place at around nine months of age, provided your child has no other medical problems that need treatment. Some children with cleft palate have a small jaw which can lead to breathing problems and may need feeding and breather tubes to help during the first year of life. For those children, repair is usually postponed until 12 months of age or once the breathing problems have resolved.
Post-surgery
Following cleft palate repair, most children stay in hospital for two to four nights. Most children will initially have some fluids and pain medicine through an intravenous drip. Once they can drink enough to stay hydrated without a drip and take oral pain medicine, they will be discharged.
Arm splints are fitted after surgery to stop the child from bending their elbows and putting their fingers in their mouths. These are worn for 10 – 21 days, depending on your surgeon’s advice. It is very important that that arm splints are always worn to stop your child poking a hole in the newly repaired palate.
Care at home
Special ‘non-sucking’ teats on squeeze bottles or open drinking cups should be used after surgery, and the surgeon will tell you how long this needs to be for. Your surgeon will advise you on what toys and food must be avoided at this time. The nursing staff will also help you with post-operative feeding techniques and can supply a bottle, non-suck teats and a written copy of the surgeon post-operative instructions.
Most children will be a little irritable in the first couple of days after surgery, but medicine will control the pain well. You may notice some pink or red saliva on the first night, and this is normal. If the hard palate has been repaired, when you look into the mouth after surgery, you will see gaps at the sides of the palate. Over the first few days, the gaps will be covered by a yellow substance and by seven to 10 days, this will be replaced by new pink healed palate tissue. You may keep seeing some food and fluid from the nose in the first few weeks, and sometimes months, after surgery until the palate mobility improves and your child gets used to using the new palate muscles.
Follow up
You will be booked for an outpatient follow up appointment to see the plastic and reconstructive surgery team between six and eight weeks after the surgery.
See your GP if your child has any problems after surgery.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Developed by Surgery (Neuro, Plastic and Reconstructive), Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS068. Reviewed: September 2018.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.