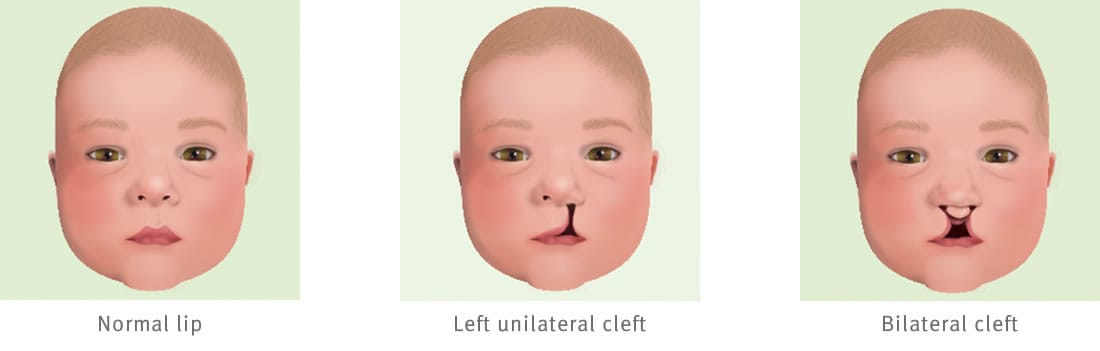
A cleft lip is a separation in the upper lip that occurs when parts of the lip do not join during pregnancy. This can occur on one side (unilateral cleft) or on both sides (bilateral cleft). Babies with cleft lips may also be born with cleft palates.
Why does it happen?
The cause of a cleft lip is unknown. It can be genetic and sometimes multiple members of the same family are born with clefts, but other times there can be no family history whatsoever.
Diagnosis
Pre-birth
If the cleft lip is picked up in a pre-natal scan, you can organise to talk to a cleft/craniofacial clinical nurse to give you some general information and answer any questions you may have.
Post-birth
If your child is diagnosed with a cleft lip at birth, you may need more time in hospital to help establish feeding. Babies born with just a cleft lip and a normal palate can usually breast feed well because breast tissue often fills the gap. However, some babies may need specialised feeding equipment such as wide-based teats and squeeze bottles. Lactation consultants, midwives and speech pathologists can all help with feeding advice. In the first few weeks of life, a cleft nurse will arrange an appointment for you and your baby to attend a multi-disciplinary cleft clinic at the hospital. Your child may also be referred to a paediatrician, an ear nose and throat (ENT) surgeon and/or an audiologist.
What is the treatment?
Surgery
Treatment for a cleft lip is not always required, however a cleft lip can be repaired surgically. The operation is usually performed when your child is between three and five months old (when their bodies can safely cope with the general anaesthetic). In some cases, this also allows time for specialists to perform orthodontic shaping to improve the position of the bone and the soft tissue before the operation, meaning the surgery outcome is better. The surgery will usually take between two to six hours, depending on the type of repair your child needs. Your child will need to stay at least one night after the surgery.
The surgery will improve both the function and appearance of the lip. After the initial reconstructive surgery, a second general anaesthetic will be needed one-week after surgery to remove the sutures used to repair the lip. This is a quick procedure and will only require a few hours’ admission to hospital.
After the surgery
Your child will stay in hospital for one or two nights after their lip repair surgery. They will probably only drink small amounts in the first 24 hours after the surgery, drinking larger amounts of the next two or three days. Intravenous fluids may be given via a drip to keep your child hydrated, and pain killers will be given as provided.
It is important to remember that it may take some time after surgery for the lip to heal fully. Scars usually tighten and pull up on the lip in the first six months after repair, making the lip look short. This should correct itself over the next six to 12 months. The scar will also probably look pink or darker in colour before it begins to fade with time. Some scars will stay a bit raised and firm for a long time before softening and flattening.
Care at home
To prevent damage to your child’s lip repair and ensure the best possible results, your surgeon will discuss with you some recommended actions and post-surgery care. These may include:
- not using a dummy
- wearing of arm splints
- insertion of nasal stents
- special feeding equipment, and/or
- diet restrictions.
Follow up
You will be booked for an outpatient appointment to see the plastic and reconstructive surgery team between four and eight weeks after the surgery to discuss scar management.
See your GP if your child has any problems following surgery.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Developed by Surgery (Neuro, Plastic and Reconstructive), Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS067. Reviewed: September 2018.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.