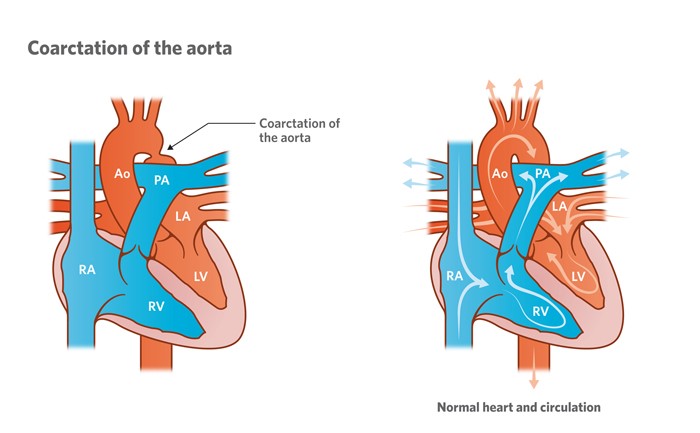
Coarctation of the aorta is a narrowing of the tube (the aorta) that carries oxygen-rich blood out of the heart to the body. If the tube is narrower than usual the heart has to pump harder. This condition can lead to high blood pressure and damaged organs in the lower body.
Signs and symptoms
The main signs and symptoms of coarctation of the aorta include:
- High blood pressure in the arms and brain.
- Excessive strain of the left ventricle of the heart.
- Damage to organs in the lower body due to lack of blood.
Diagnosis
Tests to help diagnose coarctation of the aorta include:
- Electrocardiogram (ECG) – measures the electrical activity of the heart.
- Echocardiogram (Echo) – uses sounds waves to produce a moving picture of the heart.
- CT scan – an X-ray with dye injected to highlight blood vessels.
- Cardiac catheterisation – A thin flexible tube (called a catheter) is inserted into a blood vessel in the groin and fed up into the heart to measure pressures and oxygen levels, and visualise heart structures using X-ray equipment.
These tests are usually carried out because a doctor has heard a heart murmur when examining a child with a stethoscope.
Treatment
Treatment for coarctation of the aorta depends on a child’s age, overall health, and extent of the narrowing. Procedures can include balloon dilation, stenting or surgery.
Balloon arterioplasty and stenting (via cardiac catheterisation)
A thin flexible tube with a balloon at the tip is inserted into a blood vessel in the groin and fed up into the heart. When the tip of the catheter reaches the narrow section of the aorta, the balloon is inflated to stretch the area open. Sometimes a small metal device known as a stent may be inserted to keep the aorta open. The procedure is performed under a general anaesthetic.
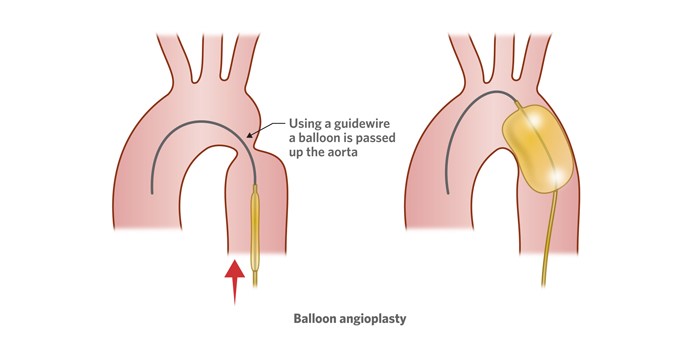
If a balloon arterioplasty or stenting is not suitable, surgery may be necessary.
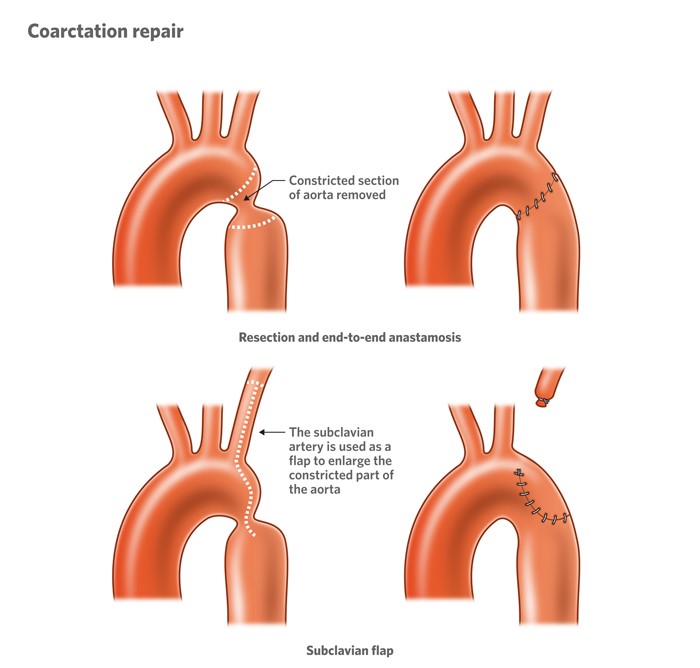
Surgical repair
In some cases, the narrow area of the aorta can be removed surgically or it can be enlarged and repaired using existing structures (an artery) of the heart or a synthetic patch. Your child’s doctor will explain the treatment options and discuss all risks with you.
Developed by Queensland Paediatric Cardiology Service, Queensland Children's Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS249. Reviewed: January 2024.
Illustrations republished with permission from The Royal Children's Hospital, Melbourne, Australia. Images subject to copyright.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.