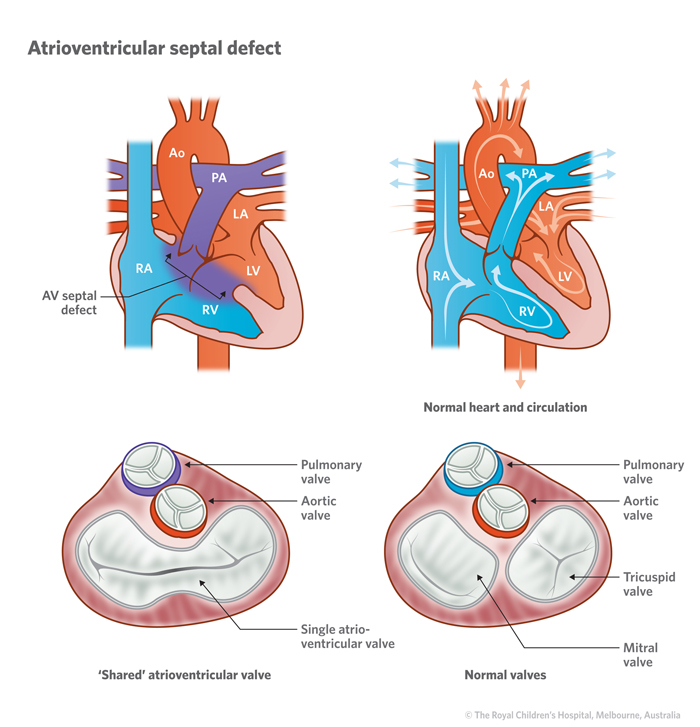
An atrioventricular septal defect (AVSD) is a complex heart condition involving more than one abnormality in the structure of the heart. Abnormalities that make up an AVSD are:
- Atrial septal defect (ASD) – a hole in the atrial septum (the wall that separates the left and right chambers (or atrium) of the heart. This allows blood to pass from one side of the heart to the other, usually from left to right which can lead to the heart enlarging on the right side and lung circulation becoming overloaded. It can also cause abnormal heart rhythms.
- Ventricular septal defect (VSD) - a hole in the wall of the heart between the pumping chambers of the heart (ventricles) which allows oxygen-rich “red” blood to pass from the left ventricle through the hole and mix with oxygen-poor “blue” blood in the right ventricle.
- Common atrio-ventricular valve – a single valve sitting between the atria and the ventricles instead of two valves. This common valve allows blood to move from the atria to the ventricles when the heart relaxes and it closes when the heart contracts. It is common for this valve to have some “leakiness” when it closes and this known as valvular incompetence or regurgitation.
Due to ASD and VSD allowing blood to flow from the left side of the heart to the right side, the heart can become bigger (dilated) and not functional correctly. The extra blood volume is pumped from the right side of the heart into the lungs, and which can damage the blood vessels in the lungs. Over time, the blood vessels in the lungs will thicken their walls, a condition called pulmonary hypertension.
Signs and symptoms
The main signs and symptoms of an atrioventricular septal defect include:
- fatigue with exertion
- pale/cool skin
- rapid breathing and/or heart rate
- poor weight gain
- feeding difficulties.
Diagnosis
Tests that help diagnose atrial septal defect include:
- Chest X-ray – to show if the heart is enlarged and if there is fluid in the lungs.
- Electrocardiogram (ECG) – measures the electrical activity of the heart.
- Echocardiogram (Echo) – uses sound waves to produce a picture of the heart.
- Cardiac catheterisation – A thin, flexible tube (called a catheter) in inserted into a blood vessel in the groin and fed up into the heart to measure pressures and oxygen levels, and visualise heart structures using X-ray equipment. The procedure is performed under a general anaesthetic. Learn more about cardiac catheterisation.
These tests are usually performed because a doctor has heard a heart murmur (turbulent blood flow) when examining a child with a stethoscope.
Treatment
Surgery is almost always necessary. Surgery involves using a patch to close the hole.
Prior to surgery, measures at home may include:
- Nutritional supplements for babies who are not growing adequately.
- Nasogastric tube feeding for babies with feeding difficulties. A small flexible tube is passed down through the baby’s nose and into the stomach and food is delivered via the tube.
- Diuretics - medicines to help relieve lung congestion.
When to seek help
See your GP or nearest hospital if your child has:
- Shortness of breath
- Easy tiring, especially after activity
- Swelling of legs, feet, or belly (abdomen)
- Sensations of a rapid, pounding heartbeat (palpitations) or skipped beats.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Developed by the Cardiology Department, Queensland Children's Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS256. Reviewed: January 2024
Illustrations republished with permission from The Royal Children's Hospital, Melbourne, Australia. Images subject to copyright.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.