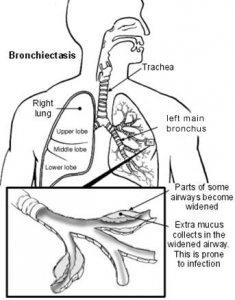
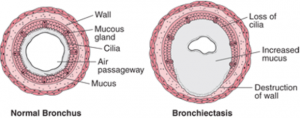
Bronchiectasis is a condition in which some of the breathing tubes (bronchi) are damaged by repeated infections and inflammation, and become wider and weaker than normal. Excessive mucus produced by the lining of the breathing tubes also results in a wet or phlegmy cough.
This situation is worsened by colds and flus (virus infections) and, particularly, exposure to cigarette smoke. During these periods bacterial infections (bronchitis and pneumonia) may also occur and children will need antibiotics and sometimes even hospitalisation for intravenous antibiotics.
Paediatric bronchiectasis differs from adult bronchiectasis in terms of causes, natural course and severity. With early detection and effective treatment the process can be halted and even reversed in children.
Possible causes of bronchiectasis
- Respiratory infections such as previous pneumonia, whooping cough, influenza, adenovirus, tuberculosis (TB) or aspergillosis (a fungal infection).
- Bronchial obstruction caused by an inhaled object (foreign body) or enlarged
lymph glands. - Hereditary conditions such as primary ciliary dyskinesia (PCD), Marfan syndrome and immuno-deficiency states, and autoimmune or hyper-immune disorders (eg. rheumatoid arthritis).
- Inhalation injury (e.g. breathing in noxious fumes or gases)
- Airway inflammation or swelling.
In up to 40 per cent of child patients, no cause may be found.
Symptoms
Bronchiectasis can develop at any age. Symptoms include chronic (lasting more than four weeks) wet or productive cough, shortness of breath, abnormal chest sounds, weakness, weight loss
and fatigue. Recurrent chest infections may produce coloured mucus. A chronic wet cough is often the only symptom present for some children with bronchiectasis.
Diagnosis
Bronchiectasis is diagnosed via a chest computed tomography (CT) scan. A chest X-ray, bronchoscopy, lung function, blood tests, sputum culture, and other tests (e.g. immune function, sweat test and genetics) for associated diseases may also be performed. Before a diagnosis of bronchiectasis is made, symptoms are often attributed to asthma or a viral infection.
If a chronic wet cough fails to respond to four weeks of appropriate antibiotics it increases the probability of underlying bronchiectasis and is an indication for referral to a specialty respiratory service.
Treatment
Treatment requires a multi-disciplinary approach with regular reviews. The aim is to control symptoms, improve quality of life and prevent disease progression. Treatment includes:
- Early use of antibiotics for acute flare-ups or epsiodes
- Daily airway clearance techniques (chest physiotherapy – see below)
- Appropriate vaccinations
- Avoiding irritants such as cigarette smoke
- Bronchodilators (only if asthma is also present)
Chest physiotherapy
Chest physiotherapy aims to mobilise, shift and clear mucus to prevent infections.
A physiotherapist will advise on the most appropriate techniques for your child’s age and disease. Techniques may include breathing exercises, chest percussion or positive expiratory pressure (PEP) devices. Regular exercise is also important.
When to seek help
See your GP if your child has any common symptoms.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Developed by the Respiratory and Sleep Unit, Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS121. Reviewed: January 2017.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.