Management
Refer to flowchart [PDF 209.81 KB] for a summary of the emergency management for a child with an inhaled foreign body:
Urgent referral to ENT team (onsite or via Retrieval Services Queensland (RSQ)) is required for children with:
- signs and symptoms of upper airway obstruction
- respiratory distress
- abnormal vital signs
- other signs and symptoms of concern to treating clinician
Prompt referral to ENT via local practices is required for stable patients requiring diagnostic or therapeutic bronchoscopy.
All patients with inhaled foreign bodies should be referred to ENT initially who will contact the respiratory team at their discretion.
Upper airway foreign body
Seek immediate senior assistance onsite (emergency/paediatric/anaesthetics/critical care/ ENT) in a child with airway concerns or inhaled button battery.
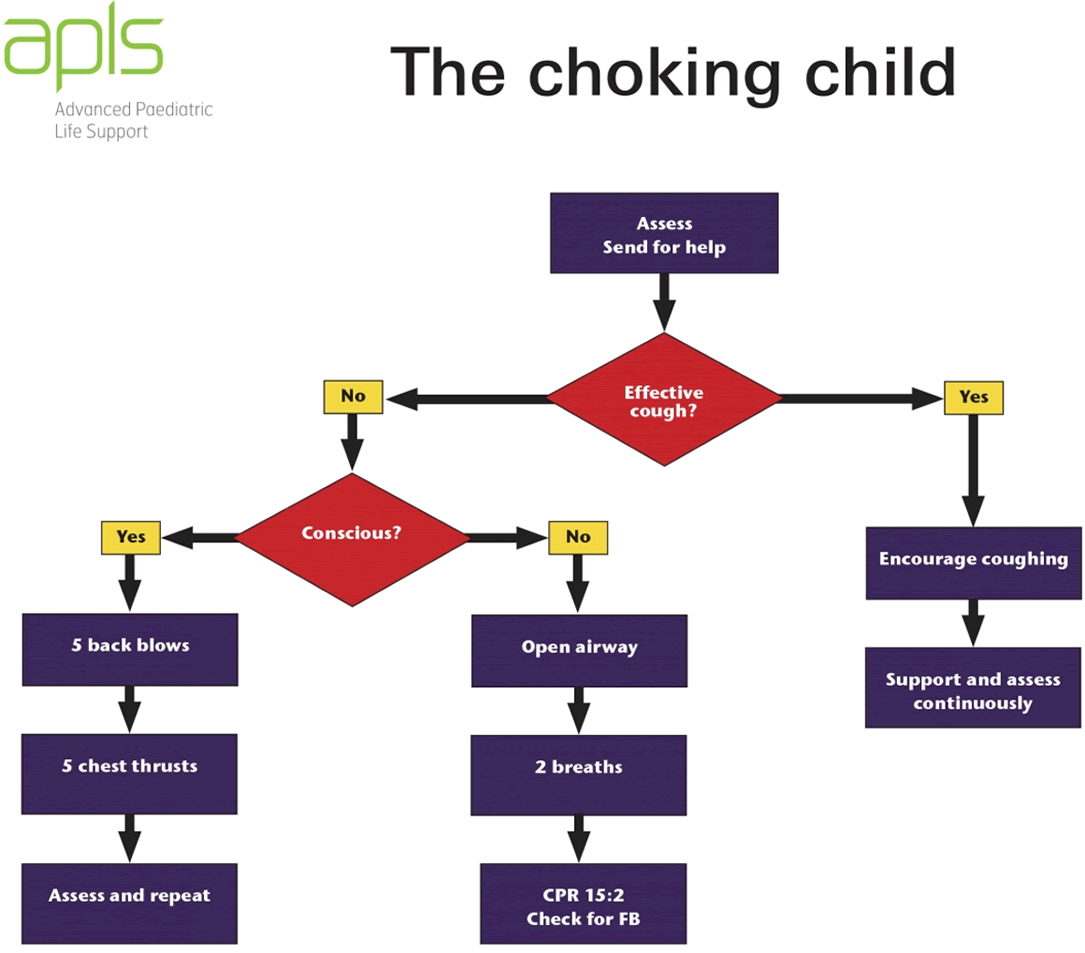
Evaluate and manage airway compromise in accordance with APLS guidelines.2
Supportive management is recommended initially in a child with no immediate airway concerns. Nurse the child in a position of comfort with cardiorespiratory monitoring and supplemental oxygen as required.
Nebulised adrenaline is not recommended due to the risk of dilation permitting distal movement of the foreign body resulting in complete airway obstruction.1
Foreign body removal with Magill forceps under direct visualisation must only be performed in controlled environments in a setting with skills and resources for advanced airway management.1
All children with suspected foreign body inhalation should be kept nil by mouth pending investigations and consultation with subspecialty teams, if required.
Apply topical amethocaine (or equivalent) in preparation for IV cannulation.
Avoid potentially distressing procedures in a child with upper airway compromise.
Lower airway foreign body
Bronchoscopy is recommended for diagnostic and/ or therapeutic purposes for the following children:
- history of foreign body inhalation and either:
- abnormal findings on physical or radiological examination or
- ongoing symptoms despite normal physical and radiological findings
- unexplained atypical/prolonged respiratory symptoms that have failed to respond standard medical therapy
Bronchoscopy is not recommended on initial presentation for children with a clear history of choking and normal physical and radiological findings as the risk of bronchoscopy is considered to exceed the risk of a retained inhaled foreign body. A bronchoscopy may be indicated if these children develop otherwise unexplained respiratory symptoms within a month of the incident.
Seek ENT advice in a child who presents with otherwise unexplained respiratory symptoms within a week of a choking episode.
Seek Paediatric Respiratory advice (if available locally), or Paediatric/ENT service as per local practice in a child who presents with otherwise unexplained respiratory symptoms more than a week after a choking episode.