Case 1 - Olivia
- You are a clinician working in an emergency department in Queensland.
- You are about see a 1 year-old female called Olivia who was brought in by her mother Elizabeth. Elizabeth tell you the reason they presented was that she thinks 'Olivia had a seizure'. The event is described as 30 seconds of arms and legs stiffening and jerking. She returned to baseline after 15 to 20 minutes.
- Observations: RR: 30 O2: 99% T: 37.1 HR: 130
- The history is notable for 1 to 2 days of rhinorrhoea, occasional dry cough, and fevers up to 38.8. Oral intake is slightly reduced. She has no relevant medical or family history. Immunisations are up to date.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Olivia appears well and is interactive. She has a red, injected pharynx with mildly inflamed tonsils. The rest of the examination, including a neurological examination, is normal. She is not clinically dehydrated.
Questions to discuss about Olivia’s case
- What is the most likely diagnosis?
- What age does this diagnosis occur?
- What are the different types of febrile convulsions?
- What tests (if any) would you request for Olivia?
- What education would you provide the family? Consider recurrence risk, relationship with epilepsy, neurological prognosis, use of paracetamol, first aid advice.
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 2 - Tania
- You are a clinician working in an emergency department in Queensland.
- You are about see a 3 year old female called Tania who was brought in by her father Felipe. Felipe tell you the reason they presented was that he thinks 'Tania had a seizure'. The event is described as 30 seconds of arms and legs stiffening and jerking. She returned to baseline after 15 to 20 minutes.
- Observations: RR: 25 O2: 99% T: 36.5 HR: 125
- Tania has recently been well, with no infective symptoms including no fever, cough, rhinorrhoea, vomiting, diarrhoea. There is no history of recent trauma. Her oral intake has been normal.
- This is her first episode.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Tania appeared well and was interactive. She was not dehydrated. There was no increased work of breathing. Her ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
Questions to discuss about Tania’s case
- What is the most likely diagnosis?
- What tests (if any) would you like to do?
- What are some differential diagnoses and underlying causes to consider for Tania’s episode?
- What is your management plan (including education) for Tania?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 3 - Kai
- You are a clinician working in an emergency department in Queensland.
- QAS has called to advise that they are soon to arrive with a 1 year old male called Kai who is actively having tonic-clonic activity for approximately 12 minutes and has not responded to one dose of buccal midazolam.
- IV access has not been successful.
- Kai has no known seizure management plan.
- You and the rest of the resuscitation team are preparing for Kai’s arrival.
Questions to discuss about Kai’s case
- When is a seizure considered status epilepticus?
- What is the next treatment you should prescribe Kai?
- If this fails, what is your next line treatment?
- What are your thoughts on phenytoin versus Keppra?
- What should you do if Kai continues to have seizures after a second line agent?
- What tests (if any) should you do?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 4 - Lydia
- You are a clinician working in an emergency department in Queensland.
- You are about see a 4 day old female called Lydia who was brought in by her foster carers Matthew and Mitchell. They tell you the reason they presented was that they think 'Lydia has been having seizures'. The event is described as brief spasms. She is sleeping during these events. They have taken a video of these events.
- Observations: RR: 50 O2: 100% T: 36.5 HR: 140
- Lydia has been well since birth, with no infective symptoms including no fever, cough, rhinorrhea, vomiting, diarrhoea. There is no history of recent trauma. Her oral intake has been normal.
- The perinatal history is uneventful.
- Lydia appeared well and was interactive. She was not clinically dehydrated. Head circumference was tracking on the 50th percentile with a normal anterior fontanelle. There was no increased work of breathing. Her ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
- Refer to Module 7 – Seizures and Toxicology - case 4 to view a video of a similar presentation.
Questions to discuss about Lydia’s case
- What is the most likely diagnosis?
- What are some differentiating features between this and epileptic events?
- What is your management?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 5 - Joe
- You are a clinician working in an emergency department in Queensland.
- You are about see a 12 month old male called Joe who was brought in by his father Bryan and mother Cassandra. Bryan and Cassandra tell you the reason they presented was that they think 'Joe had a seizure'. They have now presented to ED three times in 1 month with a similar presentation. There is a referral for an EEG and an outpatient General Paediatrician review pending.
- Observations: RR: 30 O2: 100% T: 36.5 HR: 120
- On history, the parents note that Joe was crying as he was not given his favourite toy. He cried loudly and then appeared to hold his breath, and then suddenly stopped breathing, turned blue, and became very floppy and unresponsive. The two previous presentations were similar, and involved Joe crying due to other reasons, with similar symptoms.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Joe appeared well and was interactive. He was not dehydrated. There was no increased work of breathing. His ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
- Refer to Module 7 – Seizures and Toxicology - case 5 to view a video of a similar presentation.
Questions to discuss about Joe’s case
- What is the most likely diagnosis?
- What test (if any) could you do?
- What is your management of Joe?
- What is Joe’s prognosis?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 6 - Piper
- You are a clinician working in an emergency department in Queensland.
- You are about see a 14 year old female called Piper who was brought in by her mothers Delilah and Adeline. Piper tells you the reason she presented was that she 'fainted'.
- Observations: RR: 16 O2: 100% T: 36.5 HR: 80 Systolic BP 100 No postural changes
- On history, Piper states she was walking with her friends when she started to feel dizzy, nauseous and felt her vision go 'funny'. The next thing she recalls is waking up surrounded by all of her friends and two teachers. She was able to stand up and walk to the sick bay where her mothers came to pick her up. There was no incontinence. On further history, you identify that it was a hot day and that Piper had missed breakfast and had not had much water to drink.
- A HEEADSSS assessment identified that Piper was vegetarian, with no other relevant points.
- Collateral history from one of Piper’s friends, Rachel, who was present at the time suggests that she was unconscious for only a few seconds. Rachel explains that Piper was not confused on waking and she did not see any abnormal movements at any point.
- There is no relevant past personal or family history, specifically there is no family history of cardiac death, arrhythmia, or sudden death.
- Piper appeared well and was interactive. She was not dehydrated. There was no increased work of breathing. Her ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
Questions to discuss about Piper’s case
- What is the most likely diagnosis?
- What are some causes and differential diagnoses?
- What test (if any) should you do?
- What is your management of Piper?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 7 - Himari
- You are a clinician working in an emergency department in Queensland.
- You are about see a 3 month old female called Himari who was brought in by her mother Ichika. They tell you the reason they presented was that 'Himari went floppy'.
- Observations: RR: 35 O2: 100% T: 36.5 HR: 120
- The history is notable for an event whereby Ichika was carrying Himari and she notably went very pale and floppy for a period of 5 to 10 seconds. Her breathing seemed irregular but Ichika is unable to elaborate further on this 'as it happened so fast'. She returned back to baseline following this event. Ichika is very concerned about this event. The most recent feed was 2 hours prior. She has never had similar events previously.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Himari appeared well and was interactive. She was not dehydrated. There was no increased work of breathing. She has a normal colour with no cyanosis. Her ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
Questions to discuss about Himari’s case
- What is the most likely diagnosis?
- What features made you consider this diagnosis?
- How do you determine if Himari’s event should be classified as ‘low-risk’ or ‘high-risk’?
- What is your approach to the management of Himari?
- What is your general approach to a ‘low-risk’ or ‘high-risk’ case?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 8 - Manaia
- You are a clinician working in an emergency department in Queensland.
- You are about see a 18 month old male called Manaia who was brought in by his father Kauri. He tells you the reason they presented was that 'Manaia looks pale and lethargic'.
- Observations: RR: 28 O2: 100% T: 37.4 HR: 150
- Triage glucometer BSL 2.3 Ketones 3.9
- The history is notable for 2 days of coughing, rhinorrhea and subjective fevers. Kauri ’s oral intake was reduced yesterday but today, he has not wanted to eat or drink anything for the past 12 hours. Over the day he has become more lethargic.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Manaia appeared lethargic, slightly pale but not toxic. There was no evidence of clinical dehydration. There was no increased work of breathing. His ENT examination revealed a red and inflamed pharynx. His respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
Questions to discuss about Manaia’s case
- What is the definition of hypoglycemia in children?
- What is the most common cause of hypoglycemia in children?
- What are some other causes?
- Should you investigate Manaia for an underlying disorder as a cause for his hypoglycemia?
- How would you initially manage Manaia?
- Manaia’s BSL on iSTAT was 2.4. What should you do next?
- What should be considered in the management of Manaia in the SSU/Ward setting?
- What should be done/given to Manaia prior to discharge?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 9 - Samantha
- You are a clinician working in an emergency department in Queensland.
- You are about see a 13 year old female called Samantha who was brought in by her mother Therese. They tell you the reason they presented was that 'Samantha took a bunch of pills'.
- Observations: RR: 16 O2: 100% T: 36.5 HR: 85
- There is no relevant medical history.
- Samantha appeared well and was interactive. Her ENT, respiratory, cardiovascular, abdominal, and neurological examinations were all normal.
Questions to discuss about Samantha’s case
- What should be taken on history as part of your risk assessment for Samantha?
- What are some baseline investigations to consider in a case of acute poisoning?
- What is your general approach to for the resuscitation/emergency Management for patient with poisoning? Consider an ABCD approach.
More information about Samantha’s case
Samantha identified on history that she took paracetamol tablets from the medication cabinet, and took approximately 30 tablets (500mg each) 3 hours ago. Samantha weighs 60 kg.
Questions to discuss about Samantha’s case
- Is the size of Samantha’s ingestion associated with hepatic injury?
- What tests (if any) would you request for Samantha?
More information about Samantha’s case
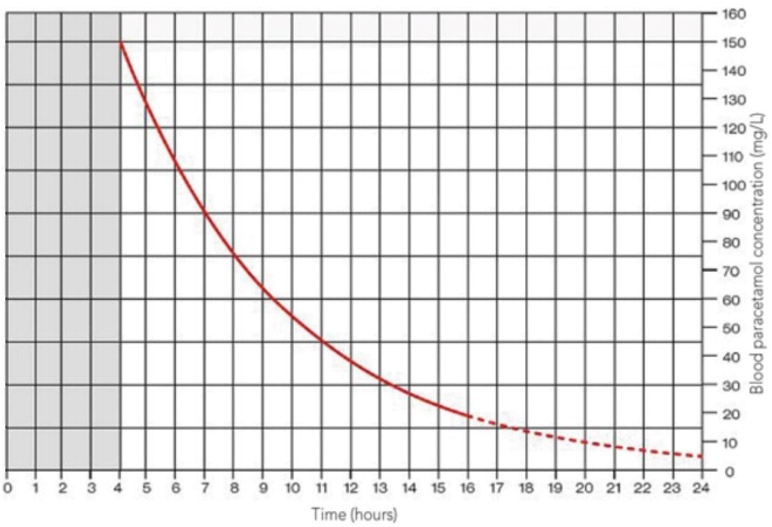
Her serum paracetamol level performed 4 hours following ingestion was 160 mg/L. Does this require further management?
Paracetamol treatment nomogram
Questions to discuss about Samantha’s case
- What are some reasons for contacting the toxicologist for advice?
- What are some indications for referral to a liver transplant unit?
- As this is a deliberate overdose, would you contact any other team?
- Would you prescribe activated charcoal for Samantha?
- Would you prescribe N-acetyl cysteine for Samantha?
- Is the management for sustained release paracetamol ingestions and repeated supratherapeutic ingestions different?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |