Case 1 - Ava
- You are a clinician working in an emergency department in Queensland.
- You are about see a 6 month old female called Ava who was brought in by her father Peter and mother Natalie. They tell you the reason they presented was that 'Ava was having difficulty breathing'.
- Observations: RR: 75 O2: 89% T: 37.2 HR: 155
- The history is notable for 3 days of rhinorrhoea, cough and subjective fevers. The work of breathing seemed to slightly increase yesterday evening, but was worse today which prompted presentation. Ava’s interest in her breastfeeds has decreased significantly since being unwell, with minimal feeds in the last 12 hours.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Ava appeared well and was interactive, but had moderate subcostal and intercostal recessions with crackles and wheeze heard bilaterally on the respiratory examination. The rest of the examination was unremarkable.
- Refer to Module 6 – Cough, crackles, and wheeze - case 1 to view a video of a similar presentation.
Questions to discuss about Ava’s case
- What is the most likely diagnosis? Consider severity and most likely etiology.
- What day does condition generally peak (and generally completely resolve)?
- What are some risk factors for severe disease?
- What investigations (if any) would you request?
- What should you consider in your management of Ava? Discuss ‘high-flow’ and its indications.
- What features in Ava should prompt you to consider that she may have cardiac disease?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 2 - Tina
- You are a clinician working in an emergency department in Queensland.
- You are about see a 2 year old female called Tina who was brought in by her single father Craig. Craig tells you the reason they presented was that 'Tina was having difficulty breathing'.
- Observations: RR: 40 O2: 94% T: 37.8 HR: 135
- The history is notable for a 3 days of rhinorrhoea, cough and subjective fevers. The breathing seemed to slightly increase yesterday evening, but was worse today which prompted presentation. Tina’s oral intake has slightly decreased since being unwell.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Tina appeared well but was noted to have difficulty breathing. She had moderate subcostal and intercostal recessions with wheeze noted bilaterally on respiratory examination. The rest of the examination was unremarkable.
Questions to discuss about Tina’s case
- What is the most likely diagnosis? Consider severity and most likely etiology.
- Will Tina go on to develop asthma? What is the difference?
- What tests (if any) should you request?
- What condition should you consider if Tina had presented with a wet cough for 4 weeks with no concerning/red flag features, with a normal examination and CXR? How would you manage this?
More information about Tina’s case
Following your initial severity assessment, you conclude that Tina’s presentation is most consistent with a presentation of a moderate episode of viral-induced wheeze.
Question to discuss about Tina’s case
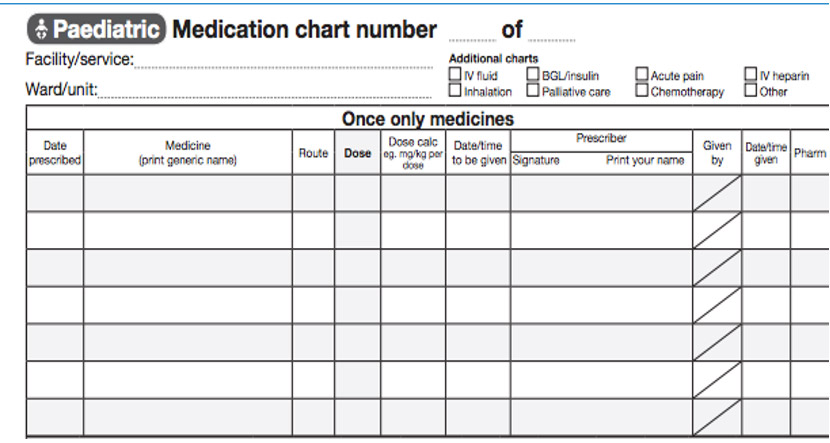
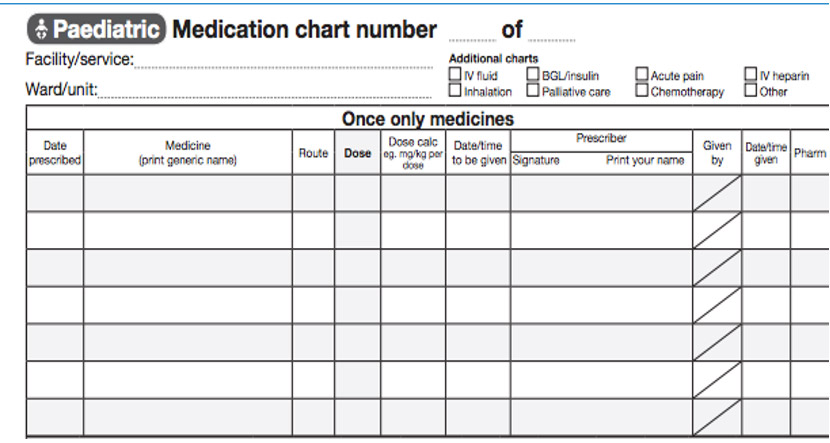
- You discuss the patient with your consultant and the decision is to proceed with a salbutamol burst. What would you chart in the medication chart shown below?
More information about Tina’s case
In addition to earlier reviews, you have now gone to review Tina at 8:40 am after the completion of her burst. You are making a decision on Tina’s response to salbutamol, and how you should stretch it.
Questions to discuss about Tina’s case
- What factors should you consider when deciding on stretching the time between salbutamol doses?
- What is salbutamol toxicity?
- Should Tina receive salbutamol using an MDI and spacer or via a nebuliser?
- What education should you give Tina's parents about how to use a spacer?
- When should you consider ipratropium bromide?
- Should you prescribe a steroid course?
- When would you consider oxygen therapy?
- When should you consider IV magnesium sulphate for Tina?
- When should you consider a preventer? Which preventer?
More information about Tina’s case
Tina has now been stretched to 3 hourly salbutamol and has been otherwise assessed as clinically suitable for discharge.
Questions to discuss about Tina’s case
- What discharge criteria should be met prior to considering discharge?
- What should the family be provided with prior to discharge?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 3 - Abraham
- You are a clinician working in an emergency department in Queensland.
- You are about see a 7 year old male called Abraham who was brought in by his mothers Peta and Stephanie. They tell you the reason they presented was that 'Abraham was having difficulty breathing'.
- Observations: RR: 35 O2: 94% T: 37.8 HR: 100
- The history is notable for 3 days of rhinorrhoea, cough and subjective fevers. The breathing seemed to slightly increase yesterday evening, but was worse today which prompted presentation. Abraham’s oral intake has slightly decreased since being unwell.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Abraham appeared well but was noted to have difficulty breathing. He had moderate subcostal and intercostal recessions with wheeze noted bilaterally on respiratory examination. The rest of the examination was unremarkable.
Questions to discuss about Abraham’s case
- What is the most likely diagnosis, including severity?
- What are some differential diagnoses to consider?
- Which tests (if any) should you request?
- How would you assess the severity of Abraham’s condition?
More information about Abraham’s case
Following your initial severity assessment, you conclude that Abraham’s presentation is most consistent with a presentation of a moderate asthma exacerbation. Abraham is 22 kg.
You discuss the patient with your consultant and the decision is to proceed with a salbutamol and ipratropium burst. There is a discussion on steroids.
Question to discuss about Abraham’s case
- What would you chart in the medication chart shown below?
More information about Abraham’s case
In addition to earlier reviews, you have now gone to review Abraham at 8:40am after the completion of his salbutamol and ipratropium burst. You are making a decision on Abraham’s response to salbutamol, and how you should stretch it.
Questions to discuss about Abraham’s case
- What factors should you consider when deciding on stretching the time between salbutamol doses?
- Which would you use for Abraham: MDI with spacer or Nebuliser? Why?
- What is the role of steroids in children with asthma? Which steroid would you prescribe?
More information about Abraham’s case
You continue to review Abraham regularly but are unable to stretch him past 45 minutely salbutamol. You feel that he is not improving to an appropriate level. He is discussed and reviewed by a senior doctor. The decision is made to move Abraham to the resuscitation zone of the emergency department. Whilst Abraham is receiving his charted medications, the decision is made to escalate his care.
Questions to discuss about Abraham’s case
- Which intravenous medication is the most suitable to prescribe at this stage?
- What are some other intravenous medications that could be used in asthma management?
More information about Abraham’s case
Abraham has now been stretched to 3 hourly salbutamol and has been otherwise assessed as clinically suitable for discharge.
Questions to discuss about Abraham’s case
- What discharge criteria should be met prior to considering discharge?
- What should the family be provided with prior to discharge?
- When would you consider a preventer for Abraham? Which preventer?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 4 - Jennifer
- You are a clinician working in an emergency department in Queensland.
- You are about see a 6 month old female called Jennifer who was brought in by her fathers William and Jonathan. They tell you the reason they presented was that '“'Jennifer was having difficulty breathing'.
- Observations: RR: 40 O2: 99% T: 37.2 HR: 155
- The initial history was that of 7 days of rhinorrhoea and cough. Over the past 2 days, this has now developed into more pronounced coughing spells. She is well between coughing fits. William tells you that Jennifer tends to vomit after the coughing episodes. Jennifer’s interest in her bottles has only slightly decreased since being unwell.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Jennifer appeared well and was interactive, with no increased work of breathing and a clear chest on respiratory examination. The rest of the examination was unremarkable.
- Refer to Module 6 – Cough, crackles, and wheeze - case 4 to view a video of a similar presentation.
Questions to discuss about Jennifer’s case
- What is the most likely diagnosis?
- How can this condition present? What are the phases?
- What tests (if any) should you do for Jennifer?
- What is your approach to the management of Jennifer?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |
Case 5 - Amin
- You are a clinician working in an emergency department in Queensland.
- You are about see a 6 month old male called Amin who was brought in by his father Mahboob and mother Aisha. They tell you the reason they presented was that 'Amin was having difficulty breathing'.
- Observations: RR: 55 O2: 86% T: 38.8 HR: 180
- The history is notable for a 24 hour history of worsening cough and fever. The difficulty with breathing seemed to get worse yesterday evening, and was not improving today which prompted presentation. Amin’s interest in breastfeeds has decreased significantly since being unwell.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- Amin appeared slightly miserable with mild lethargy. His CRT is 2 seconds with slightly dry mucous membranes. He has mild subcostal and intercostal recessions with crackles noted in the left lower zone on respiratory examination. The rest of the examination was unremarkable.
- A chest X-ray (CXR) was requested and appeared similar to the below image:
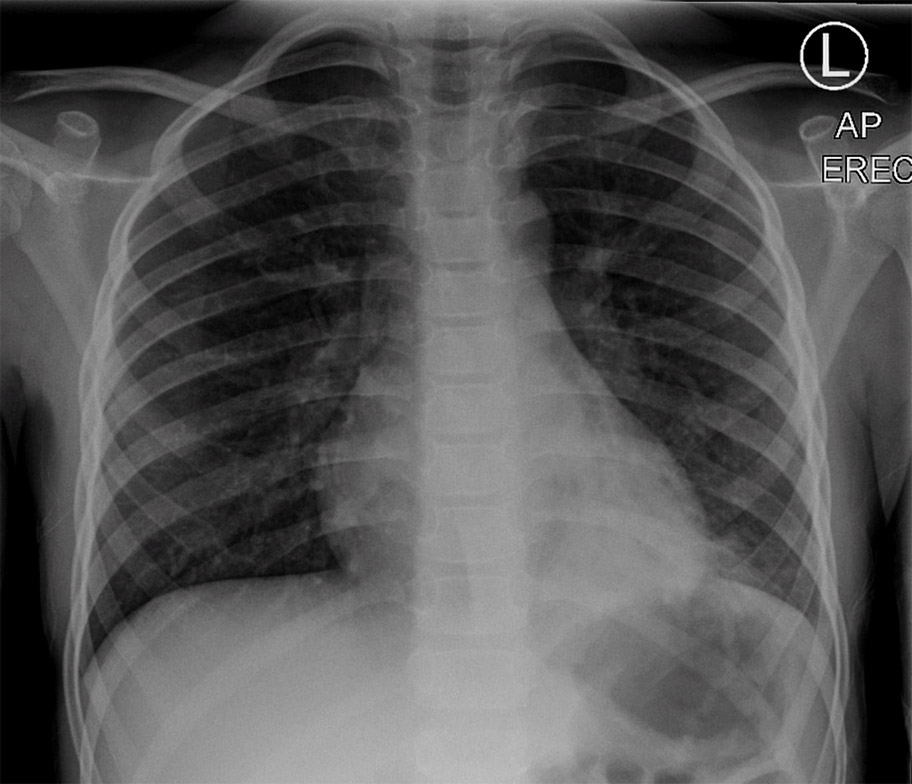
Questions to discuss about Amin’s case
- Describe the CXR.
- What is the most likely diagnosis for Amin? Consider possible etiologies, most likely bacterial etiology, and how you would classify the severity of Amin’s pneumonia.
- What investigations (if any) would you do? Are X-rays always necessary in suspected pneumonia?
- What is the most appropriate management?
More information about Amin’s case
Amin was admitted to the paediatric ward. 48 hours later, he continued to have fevers with a CRP trending from 105 mg/L on admission to 325 mg/L. A repeat CXR appeared similar to the image below.
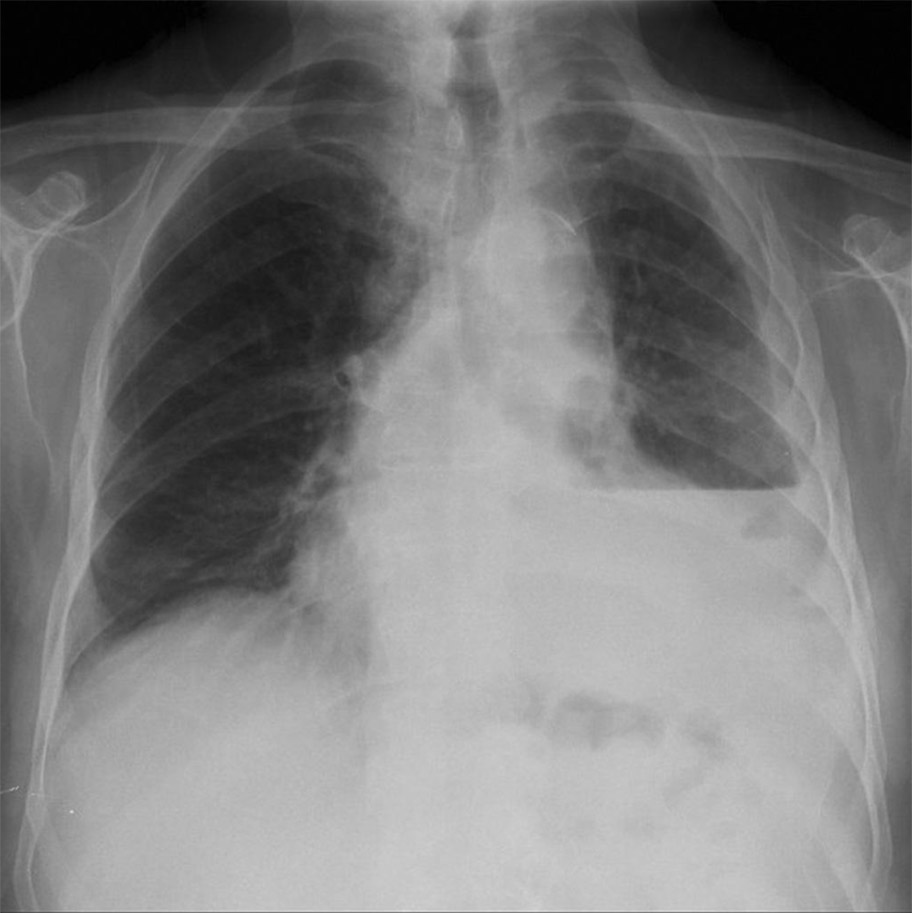
Questions to discuss about Amin’s case
- What is the most likely reason for Amin’s deterioration?
- What are some risk factors for this?
- What investigations (if any) should you do now?
- How would you manage Amin now?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |