Case 1 - Rajit
- You are a clinician working in an emergency department in Queensland.
- You are about see a 2 year old male called Rajit who was brought in by his father Thomas. They tell you the reason they presented was that 'Rajit is not moving his right arm'.
- Rajit was crossing the road 2 hours prior and holding his father’s hand. Whilst they were walking across the road, Rajit suddenly stopped and fell to the floor and so Thomas instinctively pulled him up so they could get to the other side of the road. He cried right away and has not been using his right arm since.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Rajit is not distressed. His right arm is noted to hang loosely by his side with the elbow in extension and the forearm in pronation. Any attempt you make to move his arm passively causes him distress. On distraction, you palpate the whole arm and note the absence of any neurovascular compromise, bony tenderness, deformity, or swelling.
- The image below shows a patient holding their arm held similarly to Rajit’s arm.

Questions to discuss about Rajit’s case
- What is the most likely diagnosis?
- What is a pulled elbow? Discuss anatomy and expected age group.
- What should you expect in a typical history and examination?
- When is an X-ray required/not required?
- How would you manage Rajit’s pulled elbow?
Case 2 - Madeline
- You are a clinician working in an emergency department in Queensland.
- You are about see a 5 year old female called Madeline who was brought in by her fathers Levi and Carson. They tell you the reason they presented was that 'Madeline has pain in her left arm'.
- Madeline was running in the backyard chasing her new puppy. She then tripped on a small rock and fell onto outstretched hands (FOOSH). This happened 4 hours prior. Madeline has been complaining of pain to her left wrist.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Madeline is not distressed. On palpation there is mild tenderness of the left radius but not the ulna. The elbow movement is normal. The whole left arm was examined and there was no swelling or deformity noted. Other than the radius, there was no tenderness elsewhere. There was no neurovascular compromise.
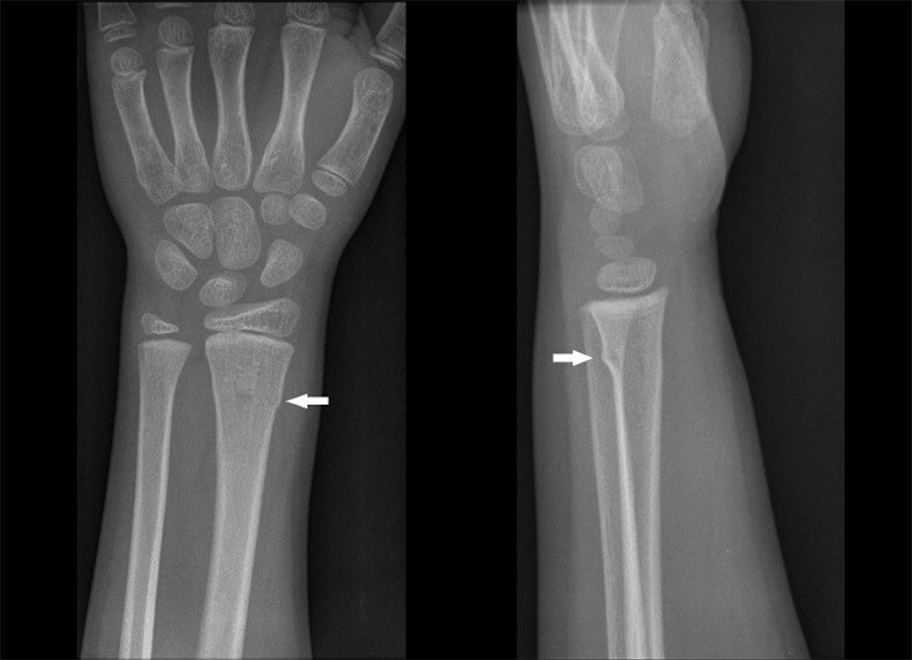
- You request an X-ray. The X-ray below is similar to Madeline’s X-ray.
Questions to discuss about Madeline’s case
- What is the most likely diagnosis?
- How would you manage this?
- Consider your management for the following minor fractures/injuries:
- Fractured clavicle.
- Occult supracondylar fracture (elevated fat pads with no obvious fracture).
- Radial head buckle fracture.
- Metatarsal fracture.
- Undisplaced non-articular fracture of finger or toes.
- Sprain to finger or toe.
- Sprained ankle.
- Patella dislocation.
- Shoulder dislocation.
- AC joint sprain.
- Buckle fracture of the proximal humerus.
- Avulsion fracture of the pelvis.
Case 3 - Stacey
- You are a clinician working in an emergency department in Queensland.
- You are about see a 9 year old female called Stacey who was brought in by her foster carer Linda. They tell you the reason they presented was that 'Stacey’s left elbow is in a lot pain and they think it's broken'.
- Stacey was climbing a tree in the backyard but then fell approximately 2 metres. She fell onto outstretched hands (FOOSH). She was in significant pain, described as 9/10. She has no other injuries. No analgesia was given as they came in straight away.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Stacey appears uncomfortable. There is limited ROM and the elbow is unable to be moved passively or actively. There is swelling noted overlying the elbow joint. There is no neurovascular compromise.
- You request an X-ray. The X-ray below is similar to Stacey’s X-ray.

Questions to discuss about Stacey’s case
- What is the diagnosis? Consider your approach to interpreting the paediatric elbow Xrays.
- How would you manage this?
Case 4 - Hugo
- You are a clinician working in an emergency department in Queensland.
- You are about see a 2 year old male Hugo who was brought in by his mother Paula. They tell you the reason they presented was that 'Hugo has not been walking since yesterday'.
- Hugo was at day care running and was then noted to fall. The specific nature of the fall is not clear. He has not been walking since. Any attempt to place Hugo on the floor by his parents has led to distress.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Hugo appears comfortable in his mother’s arms. You attempt to localise the pain. Your impression is that the pain may be coming from his right lower leg but it is difficult to be certain. There is no swelling or erythema noted. You are able to mobilise his hips with no apparent distress.
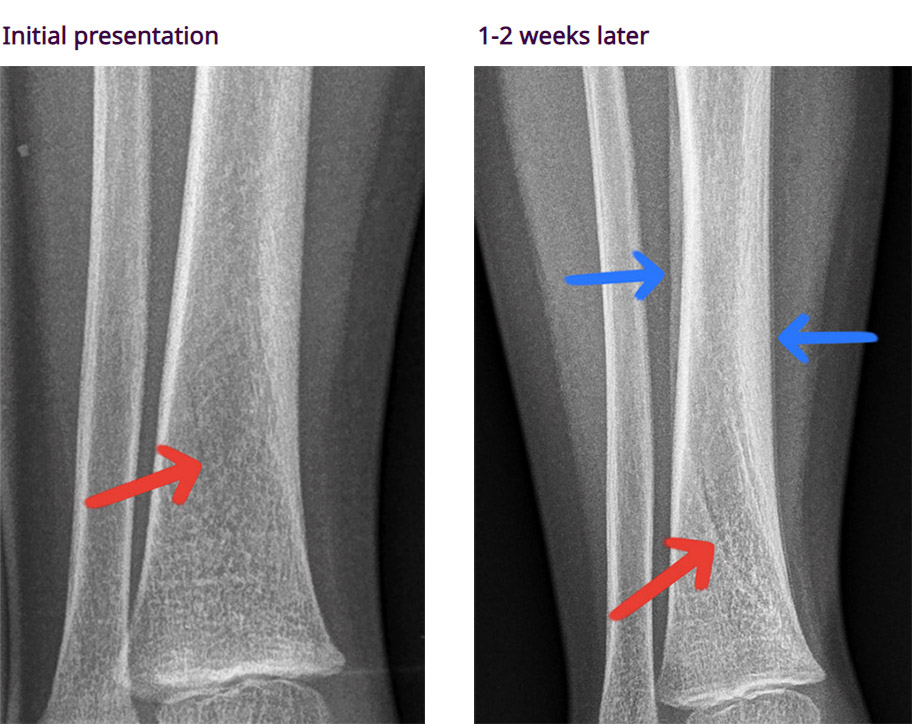
- You request an X-ray. The X-ray below is similar to Hugo’s X-ray.

Questions to discuss about Hugo’s case
- What is the most likely diagnosis? (See images and explanation of the X-ray below).
- What is a toddler fracture? Consider the type of fracture, mechanism of injury, common ages.
- How is this managed?
Case 5 - Hiroko
- You are a clinician working in an emergency department in Queensland.
- You are about see a 5 year old female, Hiroko, who presents with her father Sota. They present with concern that that 'Hiroko has been limping'.
- Hiroko has been limping for the past 24 hours. She had coryzal symptoms 5 days prior but is well now. She is able to weight bear but finds this uncomfortable. Hiroko is otherwise well with no infective symptoms. There are no B symptoms. There is no history of trauma.
- There were no relevant or concerning findings on perinatal history, developmental history, medical history, medications, allergies, vaccinations, family history, and social history.
- On examination, Hiroko appears comfortable when sitting. She is able to weight bear but has an antalgic gait. On examination, there is no bony tenderness but she has limited left hip range of motion. There is no swelling noted. The right hip is normal.
- Observations: RR: 20 O2: 100% T: 37.5 HR: 90
Questions to discuss about Hiroko’s case
- What is the most likely diagnosis? What are your differential diagnoses?
- What are some red flags to suggest serious pathology for a child with a limp?
- What investigations would you perform on Hiroko (if any)?
- If Hiroko was febrile to 39.8 degrees Celsius, what would be your provisional diagnosis and investigations?
- What is Kocher’s criteria?
Normal range for vital signs by age
| Age | Heart rate (bpm) | Minimum Systolic BP (mmHg) | Respiratory Rate (bpm) |
|---|---|---|---|
| <1 year old | 100-159 | <75 | 21-45 |
| 1-4 year old | 90-139 | <80 | 16-35 |
| 5-11 year old | 80-129 | <85 | 16-30 |
| 12-17 year old | 60-119 | <90 | 16-25 |