A shunt is a narrow tube that allows excess cerebrospinal fluid (CSF), that has built up inside the skull, to drain into another part of the body, such as the abdomen cavity (belly). The shunt is inserted through an opening in the cranium (skull) and into a part of the brain called a ventricle.
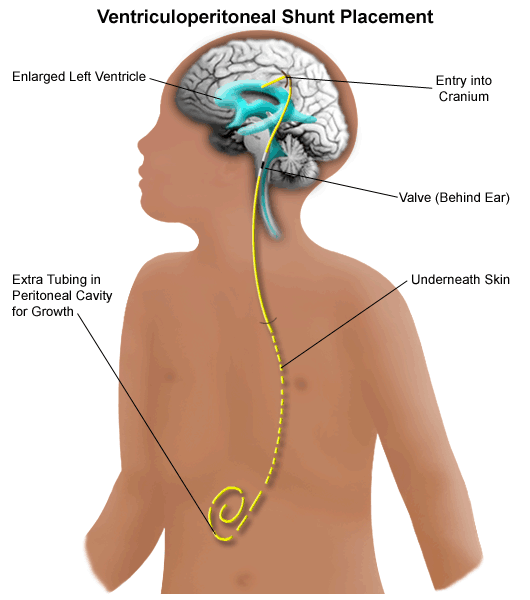
Placement of shunt in body
Shunts are named according to where they are inserted in the brain and where they exit in the body. Most shunts are ventricular to peritoneal (VP) shunts. There are also lumbar to peritoneal (LP) shunts, and ventriculoatrial (VA) shunts and ventriculo-pleural shunts. VP shunts drain fluid from the brain into the abdomen, VA drain fluid from the brain into the heart and Ventriculo- pleural shunts drain fluid from the brain into the lungs.
Shunts are made of soft, flexible tubing about 3mm in diameter. A shunt is inserted into the body by a neurosurgeon while the patient is under a general anaesthetic.
For some CSF obstructions, your neurosurgeon may make a decision to do a third ventriculostomy. This involves making a hole in the floor and sometimes the wall of the third ventricle to allow the CSF to escape.
What type of shunt will my child have?
Your child’s neurosurgeon will decide what type of shunt your child will need. In broad terms there are two types of shunts. Fixed pressure shunts have a valve that is pre-set to respond to a specific intracranial pressure such as low, medium or high.
Programmable shunts allow the neurosurgeon to set the pressure at which the valve will open, allowing it to be programmed for individual needs.
Why does my child need a shunt?
CSF is made up of water, protein, sugar and minerals and flows through four cavities, or ventricles, in the brain. Usually, CSF passes through tiny openings at the base of the brain, and then over the brain’s surface where it is absorbed into the bloodstream. It then recirculates through the bloodstream.
When there is a blockage to the flow of CSF, or the CSF cannot be absorbed, the volume of CSF builds up within the ventricles and subarachnoid space. This is called hydrocephalus. The CSF compartments may enlarge causing pressure on the brain which will be compromised if left untreated.
Hydrocephalus/CSF disorders are treated very successfully with surgical insertion of a ‘shunt’.
What happens before the operation?
Some tests (such as a CT scan, MRI or blood tests) may be required.
The neurosurgeon will explain the operation to you and ask for written consent. A shunt is inserted under a general anaesthetic. The risks associated with this surgery will be explained to you.
An anaesthetist will see your child and speak to you about when your child will need to stop eating and drinking (called fasting) in preparation for the operation.
What happens after the operation?
- Immediately after the operation, your child will either go to our intensive care unit, or direct back to the ward for close observations.
- When your child has been returned to the ward, nurses will closely observe them for the first 24 hours. This may involve waking your child at least every hour. Your child will likely be connected to a machine that monitors their heart rate and breathing. Observations will continue at a lesser frequency as your child recovers.
- If your child has had a VP shunt inserted they will have had a small section of their hair shaved.
- Your child will have a drip that will contain fluids. They will also receive pain medication for comfort.
- Your child may feel nauseous after the surgery. The nurse will monitor this and give medication if necessary. It is important to check with the nurses before you start to feed your child as they need to make sure your child is not having difficulty swallowing, and for VP shunts, that your child’s stomach is able to process food.
- It is normal for your child to be drowsy after having a general anaesthetic.
- Your child will have two dressings, one on their head and one on the site where the lower shunt tubing has been placed. For VP shunts this will be the abdomen. When the wound dressing is ready to be removed, the nurses will attend to the wound dressings in consultation with the neurosurgeon.
- If your child has an LP shunt, they will need to lie flat (or bed head at 30 degrees), usually for about 24-48 hours after the operation. The doctors will inform you when your child is allowed to sit up.
- You will be given instructions on how to look after your child’s wound before they are discharged.
What follow-up will my child need after discharge?
Your child’s neurosurgeon will see your child at a follow-up clinic about six to eight weeks after their procedure.
Important things to remember
- When the nurses do their observations they will wake your child if they are sleeping. This is necessary to assess brain function.
- Encourage your child to move their head after the shunt is inserted.
What are the signs that a shunt needs to be reviewed and/or replaced?
Problems can develop if your child’s shunt becomes blocked, disconnected or an infection develops. The signs that the shunt is not working are similar to the signs that the child has too much fluid in the brain.
If you notice any of the signs below, take your child to your closest emergency department or call 000 in an emergency.
Infants
- Poor feeding
- Vomiting
- Sleepy (hard to wake up) or not as alert
- Large head
- Bulging soft spot (fontanelle) on top of the head
- Seeming irritable (cries easily or without reason)
- Seizures
- Slowness at reaching milestones (e.g. slow to roll over or sit)
- “Sunset” eyes (when eyes appear to be always looking down and are not able to look up)
Children
- Headaches
- Nausea and vomiting
- Tired (sleeping more than usual, difficult to wake up, does not want to play as usual)
- Seeming irritable
- Change in personality, behaviours or school performance
- Loss of coordination
- Seizures
- Changes in vision
- Squint (new)
It’s important to understand, your child’s shunt may still work even if an infection is present. Signs that your child may have an infection include:
- puffiness or redness of the skin around the tube and at the incision (cut) sites
- a fever
- a stiff neck
- fluid coming out of the incision
- loss of appetite or not eating well
- generally feeling sick
- abdominal (belly) pain (for VP shunts)
When to seek urgent medical attention
Go to your nearest emergency department if you show any of signs or symptoms that a shunt needs replacing.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
In an emergency, call Triple Zero (000) and ask for an ambulance.