Asthma is a common disease of the airways – the tubes that carry air from the mouth and nose to the lungs.
During an asthma attack, the airways swell and tighten, and fill with mucus, making it hard breathe.
Asthma is one of the most common reasons children visit doctors, miss school days or are admitted to hospital
Signs and symptoms
Common signs of asthma include:
- wheezing – a whistling sound when your child breathes in and out
- heavy breathing
- shortness of breath
- a tight chest
- a cough that doesn’t go away, especially at night, early in the morning or when exercising.
Signs and symptoms may be different in every child and between asthma attacks.
Causes of asthma
Asthma can run in families and is related to other conditions, such as eczema, hay fever and allergies.
There are many things that can cause an asthma attack, including:
- a cold or chest infection
- allergy to dust mites, pollen, animal hair or smoke
- weather changes
- strong emotions, like laughing, exercising or stress.
If a child is exposed to cigarette smoke during pregnancy and early childhood, this may increase their risk of developing asthma and exacerbate attacks.
Treatment and medicines
There is no cure for asthma, but medicine can help keep it under control.
Your child’s Doctor will tell you which medicine your child should take and explain how and when to take it. They may call this an Asthma Action Plan.
Types of asthma medicine
Asthma medicines include relievers and preventers that your child breathes in, these are known as puffers. Steroids may also be used.
Relievers (e.g.Ventolin, Asmol, Bricanyl)
Your child should use a reliever as soon as they have asthma symptoms or before they exercise (if directed by your child’s doctor). Relievers:
- are used during an attack
- give relief from asthma symptoms by quickly opening the airways
- work quickly and the effects can last up to 4 hours
- are available in pharmacies. You won’t need a prescription.
Preventers (e.g.Pulmicort, Flixotide, Singulair)
Your child should use a preventer every day even if they are well. Preventers reduce swelling in the airways and will keep your child from having an asthma attack. Preventers:
- may take a few weeks to work
- are available in pharmacies. You will need a prescription from your doctor to be collected from pharmacies.
- can cause oral thrush (an infection in the mouth). Make sure your child rinses their mouth well after using a preventer to stop this from happening.
Using a spacer
Children should always use a spacer to inhale their puffer medication. A spacer is a cylinder-shaped object that helps the medicine go straight into your child’s lungs.
If your child is having a hard time using the spacer with their lips, they may have to use a mask.
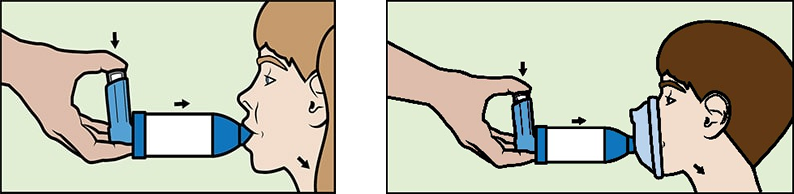
Find out how to use puffers and spacers.
Steroids
Your child should only take steroids as directed by their doctor. Steroids:
- can treat asthma symptoms in some children during and after an asthma attack
- are available in pharmacies. You will need a prescription.
Caring at home
Make sure your child knows how to take their medicine and always keep it on them. Follow your child’s Asthma Action Plan.
You can also:
- keep your child’s Asthma Action Plan nearby and share it with child's carers, daycare or school
- encourage your child to exercise (fitter children cope better with asthma attacks)
- keep them away from cigarette smoke
- ask your GP about the flu vaccine, if your child has asthma they're likely to get sicker with the flu.
When to see a doctor
See your GP if your child:
- is using the reliever at least every 3 hours for more than 24 hours.
- wakes up at night with wheezing.
The doctor will listen to your child’s chest and ask about their symptoms, allergies and family history. Older children may do a breathing test to measure how much air is getting in and out of their lungs.
If your child has been in hospital with asthma, they should see their GP within 7 days after returning home and then have regular check-ups.
Call Triple Zero (000) and ask for an ambulance if your child is:
- breathing quickly
- struggling to breathe
- trouble talking in sentences - lethargic
- pale, blue or grey.
More information
- Watch the Children’s Health Queensland asthma education videos
- National Asthma Council
Developed by the Respiratory and Emergency departments, Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS055. Reviewed: March 2023
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.